
The latest issue of the international academic journal "Nature Medicine" (Nature Medicine) published online a new study by the US Veterans Affairs (VA) St. Louis Health Care System and other teams, entitled "Long new crown after new crown breakthrough infection" ( Long COVID after breakthrough SARS-CoV-2 infection). The study, which covered 13 million people and collected data between January 1 and October 31, 2021, found that people infected with the new coronavirus after vaccination may still have symptoms associated with "long new crown" long after diagnosis. up to 6 months. These risks, as well as the risk of death, were lower than those of unvaccinated infected people, but higher than those with seasonal influenza.
"Vaccination remains critical in the fight against COVID-19. Vaccination reduces the risk of hospitalization and death from COVID-19," said study lead author and corresponding author Dr Ziyad Al-Aly of the University of Washington. It appears to provide only modest protection against long COVID." He reminded that people who have recovered from a COVID-19 breakthrough infection should continue to monitor their health, "and should see a doctor if persistent symptoms make it difficult for them to carry out their daily activities. health doctor."
It is worth mentioning that this is the first large-scale study in the world to focus on the risk of acute sequelae within 6 months after the new crown breakthrough infection. The research team analyzed the medical records of more than 13 million veterans: The records are kept in a database maintained by the U.S. Department of Veterans Affairs, the nation's largest integrated health care system. This includes 33,940 patients with new crown breakthrough infection, 4,983,491 in the control group during the same period, 5,785,273 in the historical control group, 2,566,369 in the vaccinated control group, 113,474 in the unvaccinated new crown infection, and 14,337 in the seasonal influenza group. Most of them were older white men.
As the COVID-19 pandemic continues, there is growing clinical and research evidence of long-term effects on multiple organs and systems in a substantial proportion of recovered COVID-19 patients. Previously, on May 12, a team led by Professor Cao Bin of the China-Japan Friendship Hospital and Professor Wang Jianwei of the Chinese Academy of Medical Sciences and Peking Union Medical College published the world's longest new crown patient in the "Lancet Respiratory Medicine" (Lancet Respiratory Medicine) to date. A follow-up study that provides an exhaustive analysis of the issue of "long COVID".
However, due to the mutated "nature" and immune evasion ability of the new coronavirus, the number of "breakthrough SARS-CoV-2 infection" (BTI) is also increasing globally. A so-called "breakthrough infection" is when a person who has been vaccinated has tested positive for the new coronavirus more than 14 days after completion of the vaccination, which also means that the protective barrier provided by the vaccine has been destroyed.
In the Nature Medicine study, researchers from the U.S. Veterans Affairs (VA) St. Louis Health Care System, Washington University School of Medicine and other teams refer to this "long COVID" as acute sequelae. There are currently few systematic studies worldwide reporting the increasing acute sequelae of breakthrough infections. Death and disease burden in patients with COVID-19 breakthrough infection are not trivial
Death and disease burden in patients with COVID-19 breakthrough infection are not trivial
The COVID-19 breakthrough patient here was 14 days after the first dose of Johnson & Johnson's new crown vaccine (Ad26.COV2.S) and 14 days after the second dose of the Pfizer/BioNTech vaccine (BNT162b2) or Moderna (mRNA-1273) vaccine, CARS-CoV-2 Participants who tested positive.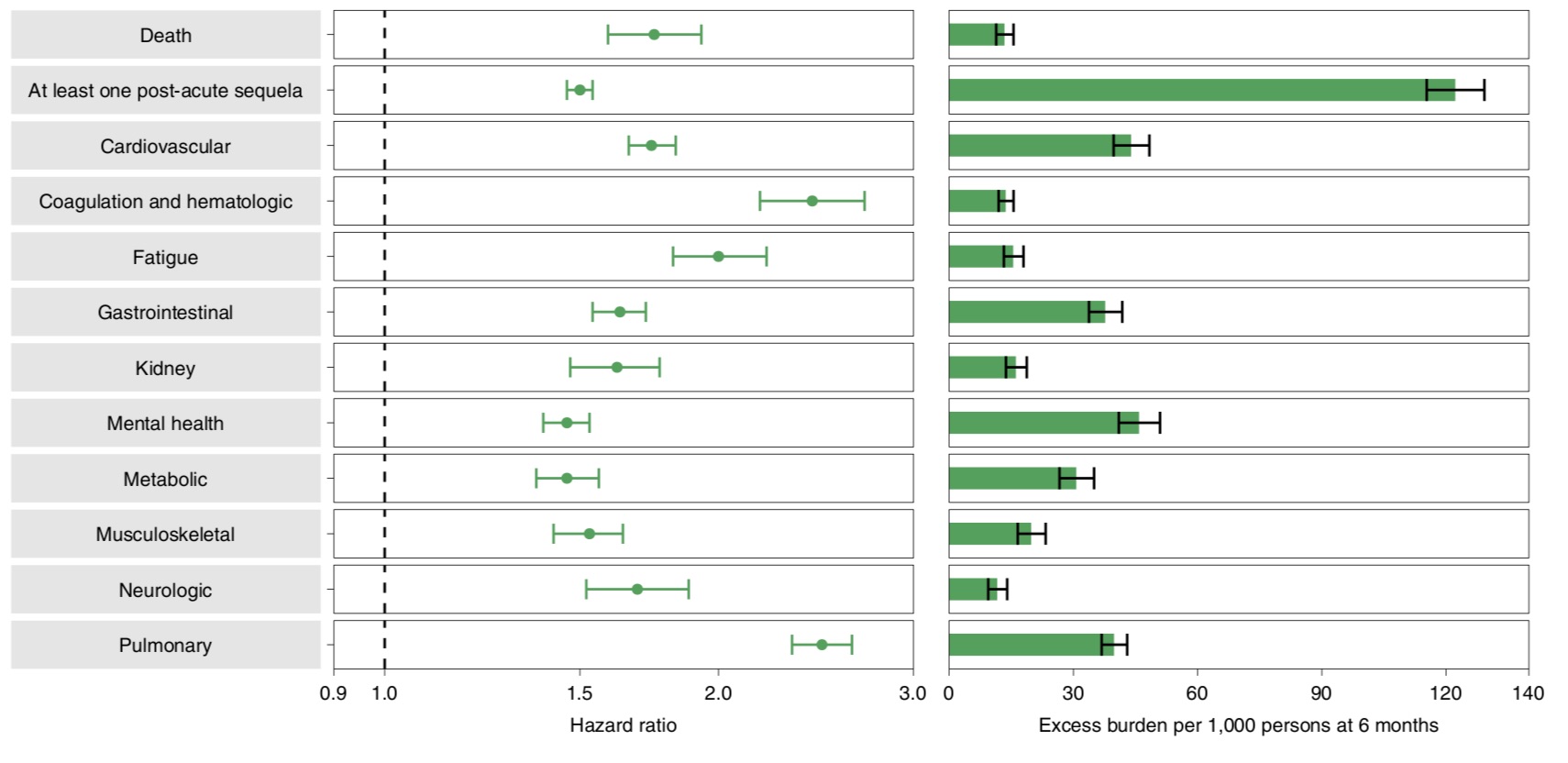
Patients with breakthrough infection also had an increased risk of at least one acute sequelae of SARS-CoV-2 (PASC) (HR=1.50, 95% CI: 1.46, 1.54; burden 122.22, 95% CI: 115.31, 129.24).
Specifically, compared with the control group in the same period, patients with breakthrough infection and then diagnosed with new coronary pneumonia developed acute pulmonary sequelae (HR=2.48; additional burden 39.82), cardiovascular disease and other extrapulmonary organ systems (HR=2.48; additional burden of 39.82) in the first 30 days. =1.74; additional burden 43.94), coagulation and hematology disorders (HR=2.43; additional burden 13.66), fatigue (HR=2.00; additional burden 15.47), gastrointestinal disease (HR=1.63; additional burden 37.68), kidney disease (HR=1.62; extra burden 16.12), mental health disorders (HR=1.46; extra burden 45.85), metabolic disorders (HR=1.46; extra burden 30.70), musculoskeletal disorders (HR=1.53; extra burden 19.81), neurological function Barriers (HR=1.69; additional burden 11.60) were all at increased risk.
The study also found that patients with breakthrough infections had an increased risk of death within 30-90 days of testing positive, and also increased, but to a lesser extent, within 90-180 days. Likewise, the risk of developing sequelae increases within 30-90 days after testing positive for SARS-CoV-2. Between 90 and 180 days after testing positive, although less risky than at 30-90 days, there is an increased risk of sequelae events, as well as an increased risk of recurrent or persistent sequelae.
In addition, patients with breakthrough infection who were not previously immunocompromised had an increased risk of death, at least one episode of PASC, and organ damage compared with controls in the same period; the risk was generally higher in previously immunocompromised patients. high. A separate analysis of patients with breakthrough infections also showed that the risk of death, at least one PASC, and organ system involvement was consistently higher in immunocompromised patients than in patients with previously uncompromised patients.
For patients with breakthrough infections, the research team also analyzed by vaccine type. The results showed that there was no statistical difference in the risk of post-acute mortality among the aforementioned three SARS-CoV-2 vaccines. However, both BNT162b2 and mRNA-1273 were associated with a reduced risk of at least one PASC (pulmonary and extrapulmonary organ involvement) compared to Ad26.COV2.S. There was no statistically significant difference in the risk of any of these outcomes between BNT162b2 and mRNA-1273.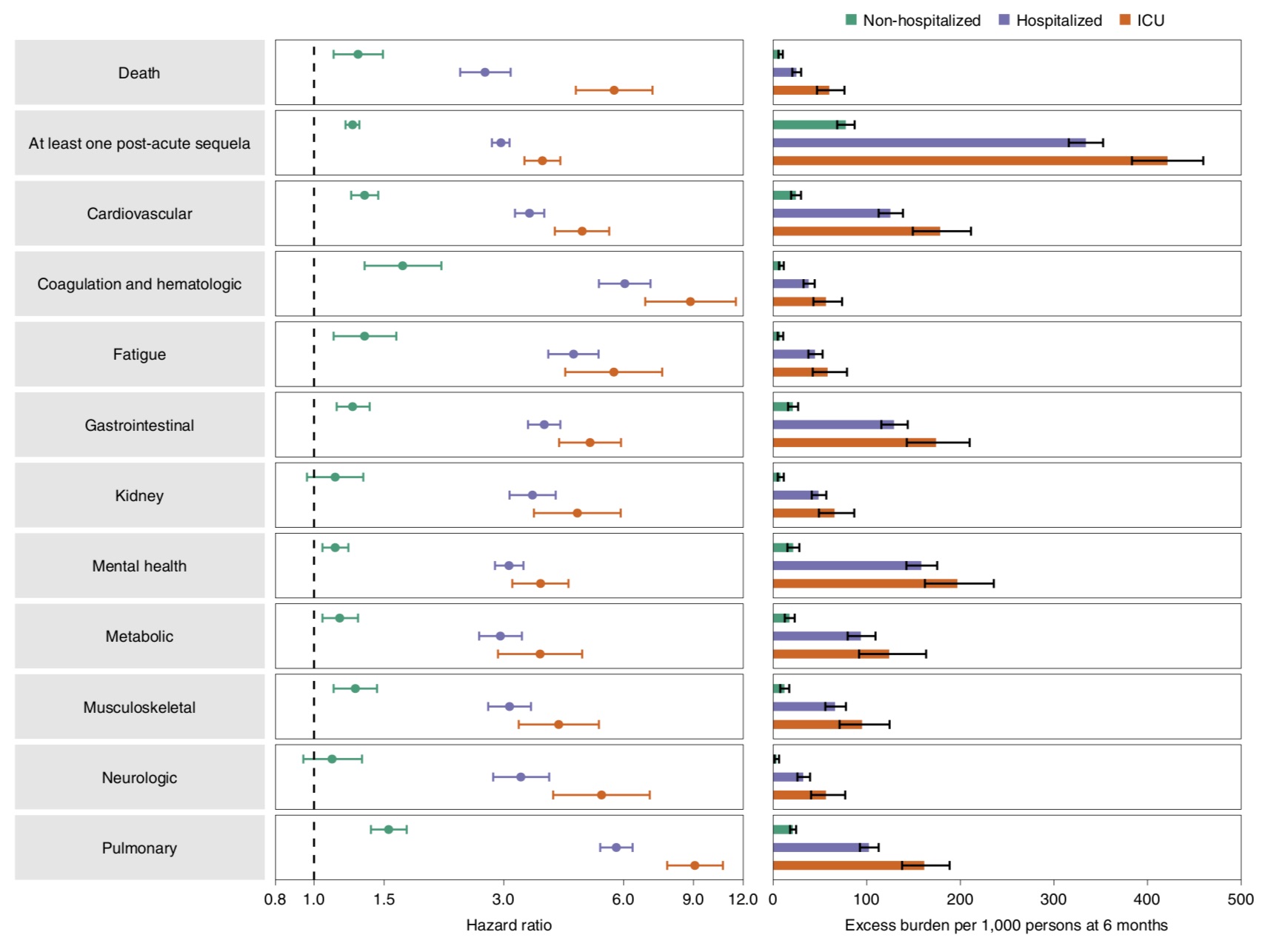
Similarly, the risk of at least one acute sequelae was significant in non-hospitalized patients (HR = 1.25 (1.20, 1.30); additional burden 77.60 (68.40, 87.04)), and further increased in the hospitalized group (HR = 2.95 (2.80, 3.10) ); additional burden was 334.10 (315.90, 352.53)), with the highest ICU burden (HR = 3.75 (3.38, 4.16); additional burden was 421.39 (383.37, 459.56)).
Notably, the research team also conducted a comparative analysis to better understand how patients hospitalized with breakthrough infections (n=3667) compared with those hospitalized with seasonal influenza (n=14337).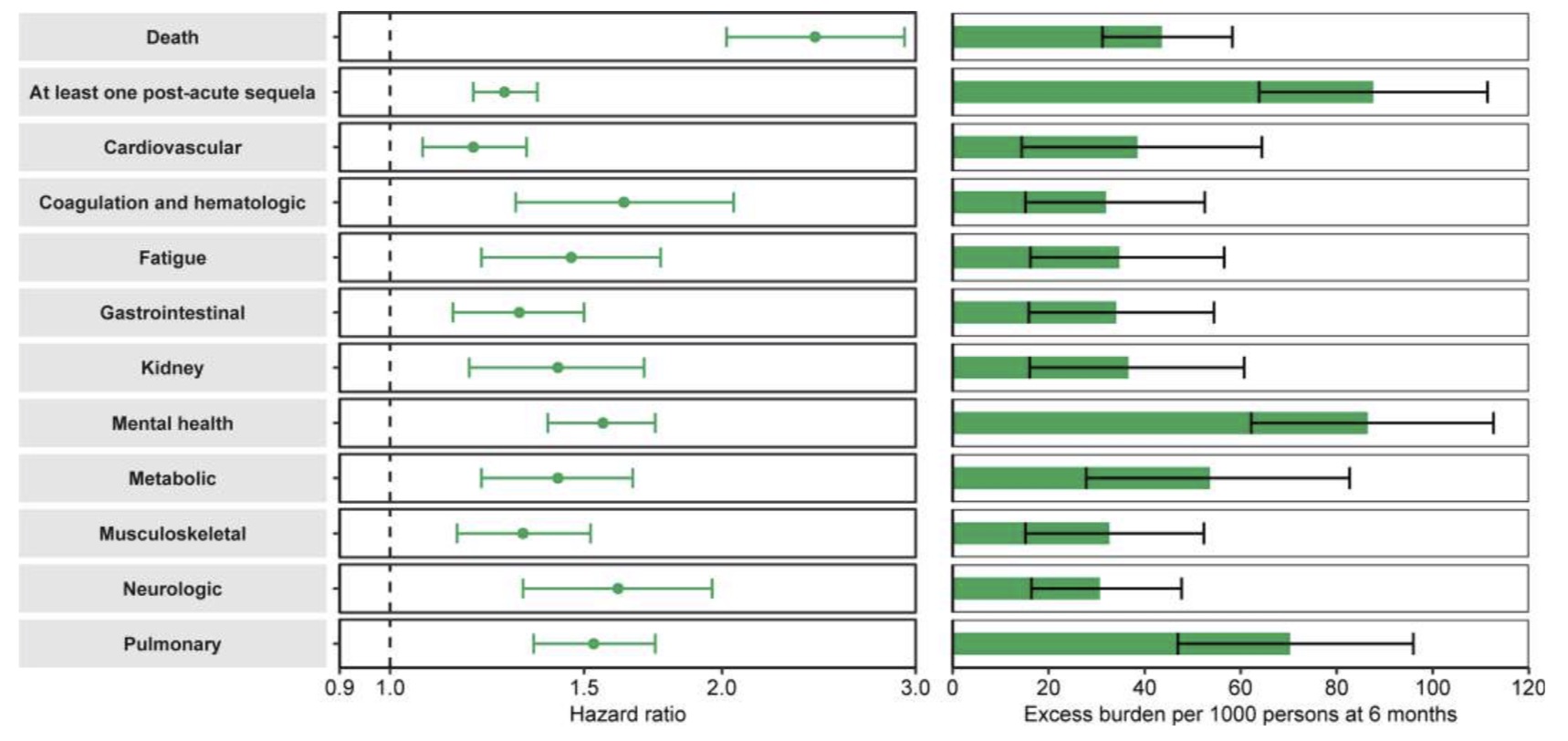 The results showed that compared with patients hospitalized for seasonal influenza, patients with new coronary breakthrough infection who were hospitalized in the acute phase of the disease had a higher risk of death within 30 days of infection (HR=2.43 (2.02, 2.93); additional burden 43.58 (31.21 , 58.26)), and an increased risk of at least one acute sequelae (HR=1.27 (1.19, 1.36); additional burden 87.59 (63.83, 111.40)).
The results showed that compared with patients hospitalized for seasonal influenza, patients with new coronary breakthrough infection who were hospitalized in the acute phase of the disease had a higher risk of death within 30 days of infection (HR=2.43 (2.02, 2.93); additional burden 43.58 (31.21 , 58.26)), and an increased risk of at least one acute sequelae (HR=1.27 (1.19, 1.36); additional burden 87.59 (63.83, 111.40)).
In addition, patients with breakthrough Covid-19 infection also showed a greater risk of sequelae in all organ systems examined compared with patients with seasonal influenza.
The research team concluded that this study showed an increased risk of death within 30 days of infection and an increased risk of acute sequelae in the lungs and several extrapulmonary organ systems in individuals with breakthrough Covid-19 infection compared with uninfected controls over the same period. The risk of death and acute sequelae was evident in non-hospitalized patients, while the risk of death and acute sequelae was further increased in hospitalized patients, with the highest risk in patients admitted to the ICU during the acute phase of the disease.
The research team emphasizes that these findings suggest that the death and disease burden experienced by patients with breakthrough Covid-19 infections is not trivial. "Our comparative analysis provides a framework to better assess and understand the risk of post-viral conditions in patients with breakthrough infection versus uninfected controls, unvaccinated SARS-CoV-2 infection, and patients with seasonal influenza."
Vaccines alone cannot minimize long-term health effects of COVID-19
They argue that the findings suggest that vaccination only partially reduces the risk of death and acute sequelae, suggesting that relying on vaccines as the only mitigation strategy may not optimally reduce the risk of long-term health consequences of SARS-CoV-2 infection. "Our findings underscore the need to continue optimizing strategies for primary prevention of breakthrough infections and will inform post-acute care for patients with breakthrough infections."
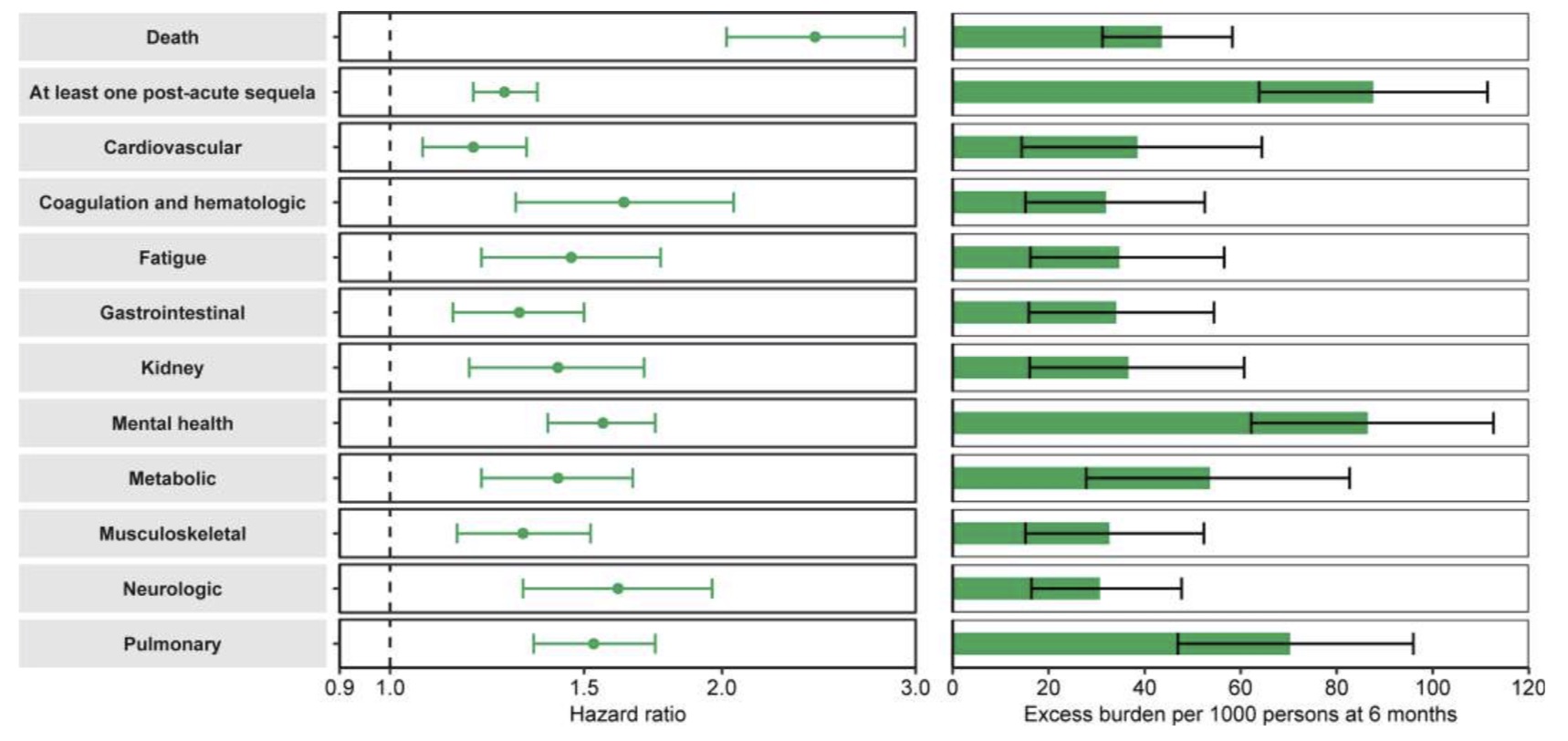
The research team pointed out that the analysis of patients with new crown breakthrough infection and unvaccinated SARS-CoV-2 infection showed that, by contrast, patients with breakthrough infection had lower risks of death and acute sequelae than unvaccinated patients. SARS-CoV-2 infected patients. These results suggest that while vaccination may reduce the risk of post-acute mortality and disease to some extent, to most effectively reduce this burden, a continued focus on primary prevention of SARS-CoV-2 breakthrough infection is required , and make this the goal of public health policy.
They caution that, given the scale of the COVID-19 pandemic and the potential for continued accumulation of breakthrough cases, the overall burden of death and disease following a breakthrough infection could be substantial. This will further add to the toll from the pandemic and will place additional pressure on an already overwhelmed health system.
The study recommends that governments and health systems should consider the care needs of patients with acute sequelae of breakthrough infections when planning and developing health resources.
The research team finally re-emphasized that prevention of SARS-CoV-2 infection and breakthrough infection are equally important. Because this study shows that patients with new crown breakthrough infection have a higher risk of acute sequelae than patients with seasonal flu. Previous studies have also given evidence that people infected with SARS-CoV-2 have a higher risk of acute sequelae than patients with seasonal influenza.
Dr. Ziyad Al-Aly cautioned, “Our current practice is likely to leave large numbers of people with chronic and potentially disabling diseases for which there is no cure. This affects not only people’s health, but their work capacity, life expectancy, economic productivity and social welfare. We need a frank national conversation about the consequences of our current practices.”
"Vaccination remains critical in the fight against COVID-19. Vaccination reduces the risk of hospitalization and death from COVID-19," said study lead author and corresponding author Dr Ziyad Al-Aly of the University of Washington. It appears to provide only modest protection against long COVID." He reminded that people who have recovered from a COVID-19 breakthrough infection should continue to monitor their health, "and should see a doctor if persistent symptoms make it difficult for them to carry out their daily activities. health doctor."
It is worth mentioning that this is the first large-scale study in the world to focus on the risk of acute sequelae within 6 months after the new crown breakthrough infection. The research team analyzed the medical records of more than 13 million veterans: The records are kept in a database maintained by the U.S. Department of Veterans Affairs, the nation's largest integrated health care system. This includes 33,940 patients with new crown breakthrough infection, 4,983,491 in the control group during the same period, 5,785,273 in the historical control group, 2,566,369 in the vaccinated control group, 113,474 in the unvaccinated new crown infection, and 14,337 in the seasonal influenza group. Most of them were older white men.
As the COVID-19 pandemic continues, there is growing clinical and research evidence of long-term effects on multiple organs and systems in a substantial proportion of recovered COVID-19 patients. Previously, on May 12, a team led by Professor Cao Bin of the China-Japan Friendship Hospital and Professor Wang Jianwei of the Chinese Academy of Medical Sciences and Peking Union Medical College published the world's longest new crown patient in the "Lancet Respiratory Medicine" (Lancet Respiratory Medicine) to date. A follow-up study that provides an exhaustive analysis of the issue of "long COVID".
However, due to the mutated "nature" and immune evasion ability of the new coronavirus, the number of "breakthrough SARS-CoV-2 infection" (BTI) is also increasing globally. A so-called "breakthrough infection" is when a person who has been vaccinated has tested positive for the new coronavirus more than 14 days after completion of the vaccination, which also means that the protective barrier provided by the vaccine has been destroyed.
In the Nature Medicine study, researchers from the U.S. Veterans Affairs (VA) St. Louis Health Care System, Washington University School of Medicine and other teams refer to this "long COVID" as acute sequelae. There are currently few systematic studies worldwide reporting the increasing acute sequelae of breakthrough infections.
 Death and disease burden in patients with COVID-19 breakthrough infection are not trivial
Death and disease burden in patients with COVID-19 breakthrough infection are not trivialThe COVID-19 breakthrough patient here was 14 days after the first dose of Johnson & Johnson's new crown vaccine (Ad26.COV2.S) and 14 days after the second dose of the Pfizer/BioNTech vaccine (BNT162b2) or Moderna (mRNA-1273) vaccine, CARS-CoV-2 Participants who tested positive.
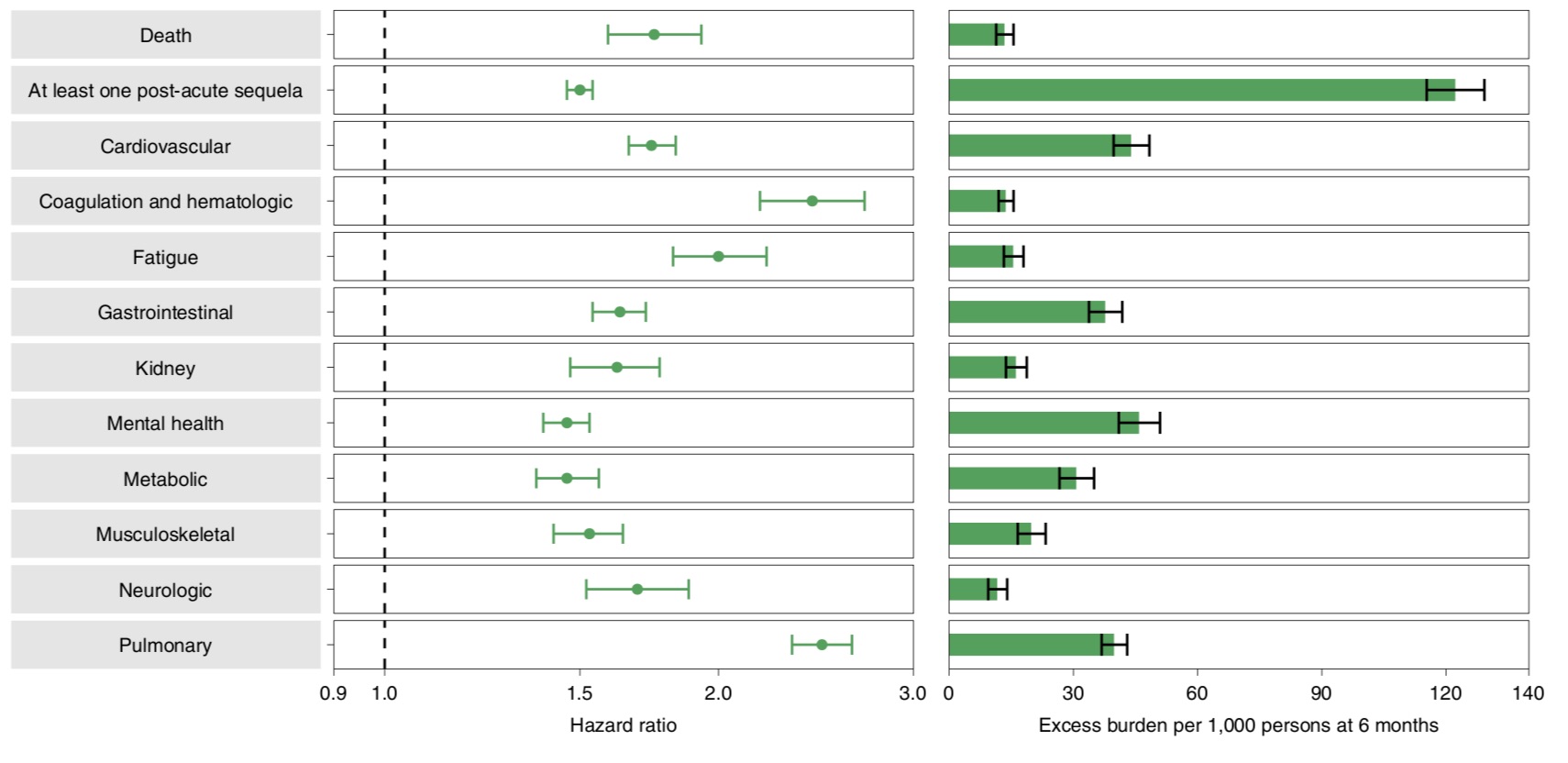
Risk of acute sequelae and additional burden at 6-month follow-up in patients with novel coronavirus breakthrough infection compared with controls in the same period.
The study found that compared with the control group of the same period, patients with breakthrough infection and subsequent diagnosis of new coronary pneumonia had an increased risk of death in the first 30 days ((hazard ratio = 1.75, 95% CI: 1.59, 1.93), and at follow-up 6 The additional burden of death for patients with breakthrough infections was estimated to be 13.36 (95% CI: 11.36, 15.55) per 1000 at 12 months, or 13.36 per 1000; all other additional health burdens increased similarly .Patients with breakthrough infection also had an increased risk of at least one acute sequelae of SARS-CoV-2 (PASC) (HR=1.50, 95% CI: 1.46, 1.54; burden 122.22, 95% CI: 115.31, 129.24).
Specifically, compared with the control group in the same period, patients with breakthrough infection and then diagnosed with new coronary pneumonia developed acute pulmonary sequelae (HR=2.48; additional burden 39.82), cardiovascular disease and other extrapulmonary organ systems (HR=2.48; additional burden of 39.82) in the first 30 days. =1.74; additional burden 43.94), coagulation and hematology disorders (HR=2.43; additional burden 13.66), fatigue (HR=2.00; additional burden 15.47), gastrointestinal disease (HR=1.63; additional burden 37.68), kidney disease (HR=1.62; extra burden 16.12), mental health disorders (HR=1.46; extra burden 45.85), metabolic disorders (HR=1.46; extra burden 30.70), musculoskeletal disorders (HR=1.53; extra burden 19.81), neurological function Barriers (HR=1.69; additional burden 11.60) were all at increased risk.
The study also found that patients with breakthrough infections had an increased risk of death within 30-90 days of testing positive, and also increased, but to a lesser extent, within 90-180 days. Likewise, the risk of developing sequelae increases within 30-90 days after testing positive for SARS-CoV-2. Between 90 and 180 days after testing positive, although less risky than at 30-90 days, there is an increased risk of sequelae events, as well as an increased risk of recurrent or persistent sequelae.
In addition, patients with breakthrough infection who were not previously immunocompromised had an increased risk of death, at least one episode of PASC, and organ damage compared with controls in the same period; the risk was generally higher in previously immunocompromised patients. high. A separate analysis of patients with breakthrough infections also showed that the risk of death, at least one PASC, and organ system involvement was consistently higher in immunocompromised patients than in patients with previously uncompromised patients.
For patients with breakthrough infections, the research team also analyzed by vaccine type. The results showed that there was no statistical difference in the risk of post-acute mortality among the aforementioned three SARS-CoV-2 vaccines. However, both BNT162b2 and mRNA-1273 were associated with a reduced risk of at least one PASC (pulmonary and extrapulmonary organ involvement) compared to Ad26.COV2.S. There was no statistically significant difference in the risk of any of these outcomes between BNT162b2 and mRNA-1273.
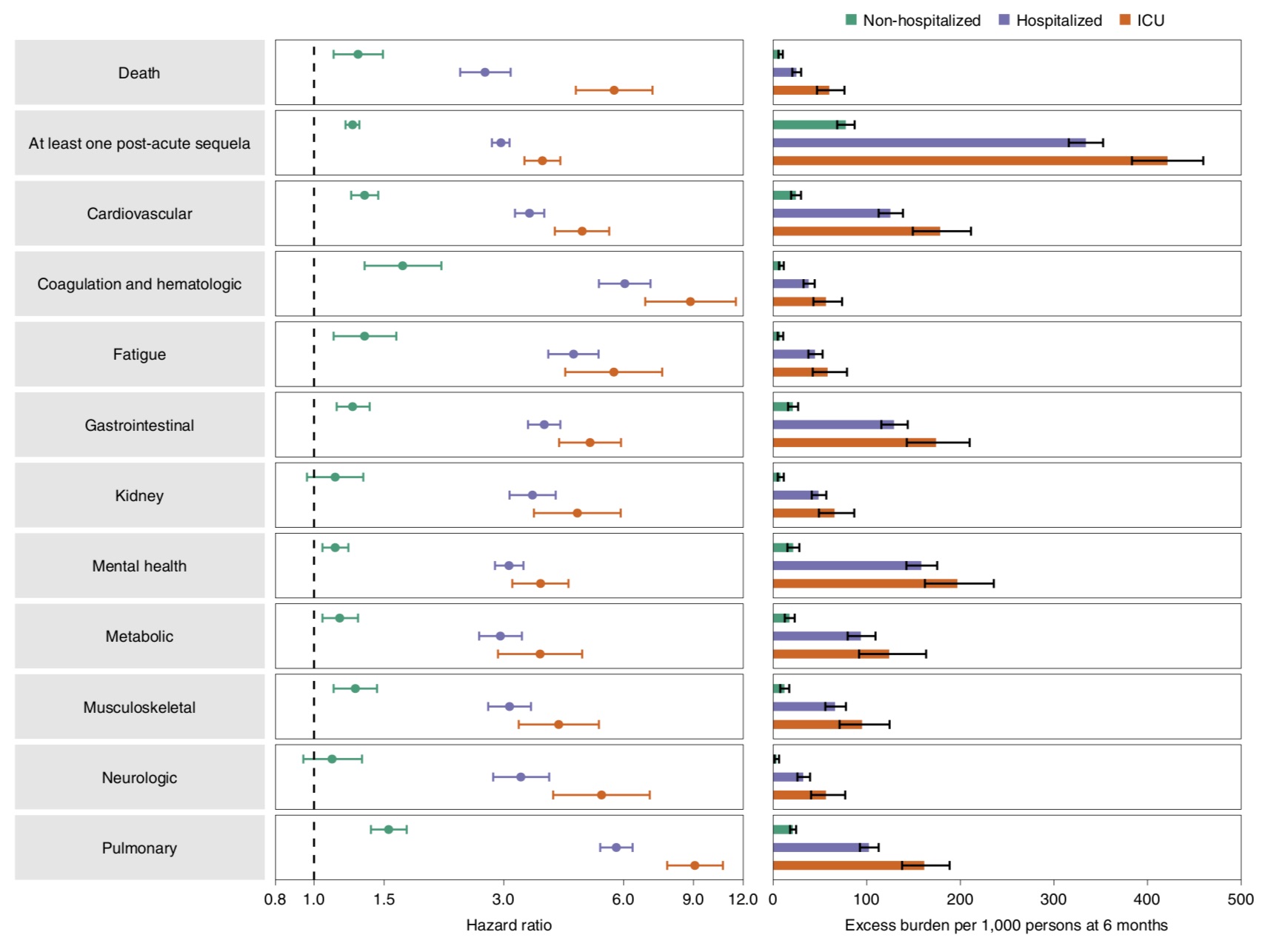
Risk of acute sequelae and additional burden of 6-month follow-up in patients with novel coronavirus breakthrough infection under various acute-phase care.
In the analysis of medical care such as hospitalization, patients with breakthrough infection had an increased risk of death within 30 days of infection, compared with controls without evidence of SARS-CoV-2 infection (HR=1.29 (1.12, 1.49). ); additional burden was 7.77 (5.62, 10.24)), and the risk was further increased in hospitalized patients (HR = 2.69 (2.33, 3.12); additional burden was 24.79 (20.39, 29.86)), and ICU hospitalized patients had the highest risk (HR = 5.68 ( 4.55, 7.09); the additional burden is 60.02(46.85, 76.19)).Similarly, the risk of at least one acute sequelae was significant in non-hospitalized patients (HR = 1.25 (1.20, 1.30); additional burden 77.60 (68.40, 87.04)), and further increased in the hospitalized group (HR = 2.95 (2.80, 3.10) ); additional burden was 334.10 (315.90, 352.53)), with the highest ICU burden (HR = 3.75 (3.38, 4.16); additional burden was 421.39 (383.37, 459.56)).
Notably, the research team also conducted a comparative analysis to better understand how patients hospitalized with breakthrough infections (n=3667) compared with those hospitalized with seasonal influenza (n=14337).
 The results showed that compared with patients hospitalized for seasonal influenza, patients with new coronary breakthrough infection who were hospitalized in the acute phase of the disease had a higher risk of death within 30 days of infection (HR=2.43 (2.02, 2.93); additional burden 43.58 (31.21 , 58.26)), and an increased risk of at least one acute sequelae (HR=1.27 (1.19, 1.36); additional burden 87.59 (63.83, 111.40)).
The results showed that compared with patients hospitalized for seasonal influenza, patients with new coronary breakthrough infection who were hospitalized in the acute phase of the disease had a higher risk of death within 30 days of infection (HR=2.43 (2.02, 2.93); additional burden 43.58 (31.21 , 58.26)), and an increased risk of at least one acute sequelae (HR=1.27 (1.19, 1.36); additional burden 87.59 (63.83, 111.40)).In addition, patients with breakthrough Covid-19 infection also showed a greater risk of sequelae in all organ systems examined compared with patients with seasonal influenza.
The research team concluded that this study showed an increased risk of death within 30 days of infection and an increased risk of acute sequelae in the lungs and several extrapulmonary organ systems in individuals with breakthrough Covid-19 infection compared with uninfected controls over the same period. The risk of death and acute sequelae was evident in non-hospitalized patients, while the risk of death and acute sequelae was further increased in hospitalized patients, with the highest risk in patients admitted to the ICU during the acute phase of the disease.
The research team emphasizes that these findings suggest that the death and disease burden experienced by patients with breakthrough Covid-19 infections is not trivial. "Our comparative analysis provides a framework to better assess and understand the risk of post-viral conditions in patients with breakthrough infection versus uninfected controls, unvaccinated SARS-CoV-2 infection, and patients with seasonal influenza."
Vaccines alone cannot minimize long-term health effects of COVID-19
They argue that the findings suggest that vaccination only partially reduces the risk of death and acute sequelae, suggesting that relying on vaccines as the only mitigation strategy may not optimally reduce the risk of long-term health consequences of SARS-CoV-2 infection. "Our findings underscore the need to continue optimizing strategies for primary prevention of breakthrough infections and will inform post-acute care for patients with breakthrough infections."
The research team pointed out that the analysis of patients with new crown breakthrough infection and unvaccinated SARS-CoV-2 infection showed that, by contrast, patients with breakthrough infection had lower risks of death and acute sequelae than unvaccinated patients. SARS-CoV-2 infected patients. These results suggest that while vaccination may reduce the risk of post-acute mortality and disease to some extent, to most effectively reduce this burden, a continued focus on primary prevention of SARS-CoV-2 breakthrough infection is required , and make this the goal of public health policy.
They caution that, given the scale of the COVID-19 pandemic and the potential for continued accumulation of breakthrough cases, the overall burden of death and disease following a breakthrough infection could be substantial. This will further add to the toll from the pandemic and will place additional pressure on an already overwhelmed health system.
The study recommends that governments and health systems should consider the care needs of patients with acute sequelae of breakthrough infections when planning and developing health resources.
The research team finally re-emphasized that prevention of SARS-CoV-2 infection and breakthrough infection are equally important. Because this study shows that patients with new crown breakthrough infection have a higher risk of acute sequelae than patients with seasonal flu. Previous studies have also given evidence that people infected with SARS-CoV-2 have a higher risk of acute sequelae than patients with seasonal influenza.
Dr. Ziyad Al-Aly cautioned, “Our current practice is likely to leave large numbers of people with chronic and potentially disabling diseases for which there is no cure. This affects not only people’s health, but their work capacity, life expectancy, economic productivity and social welfare. We need a frank national conversation about the consequences of our current practices.”
Related Posts
0 Comments
Write A Comments