Many children in Taiwan, my country, have developed encephalitis after being infected with the new crown. As of June 7, a total of 39 severe cases of COVID-19 among children under the age of 12 in Taiwan have been reported, including 17 cases of encephalitis, 8 cases of pneumonia, 3 cases of sepsis, and 4 cases of asthma, of which 17 died.
Wang Juneng, director of the Pediatric Thoracic and Intensive Care Department of Chengda University Hospital, said that children diagnosed on the island have suffered from many neurological severe diseases, especially severe encephalopathy, acute encephalitis, and explosive cerebral edema, which are relatively rare in overseas experience. The world needs to explore the reasons behind it.
In fact, it is not "uncommon overseas experience" for children to develop encephalitis after being infected with the new coronavirus. A reporter from The Paper (www.thepaper.cn) flipped through the international journal "Journal of Pediatrics" in the field of pediatrics and found that its latest issue included a study on central nervous system inflammation in children after COVID-19 infection.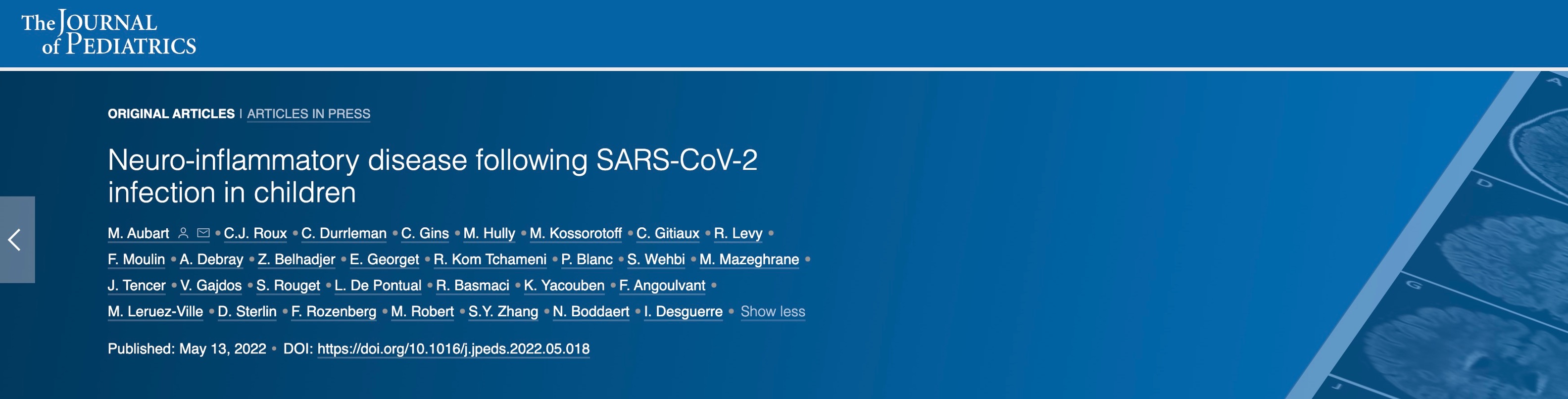 The aforementioned study collected 19 cases of children with central nervous complications after infection with Covid-19 who were referred to the Necker-Enfants Malades Hospital from 12 hospitals in the Paris region. The research team includes the Department of Pediatric Neurology, Necker-Enfants Malades Hospital, University of Paris, France, the Department of Pediatrics, Lecoudre Louis Pasteur Hospital, France, the Department of Pediatrics, CHIPS Hospital, Poissy, France, and the Department of Immunology, Pitié-Salpétrière Hospital, Sorbonne University, France, and Rockefeller, New York, USA. St. Giles Laboratory of Infectious Diseases Human Genetics, University of Rockefeller, et al.
The aforementioned study collected 19 cases of children with central nervous complications after infection with Covid-19 who were referred to the Necker-Enfants Malades Hospital from 12 hospitals in the Paris region. The research team includes the Department of Pediatric Neurology, Necker-Enfants Malades Hospital, University of Paris, France, the Department of Pediatrics, Lecoudre Louis Pasteur Hospital, France, the Department of Pediatrics, CHIPS Hospital, Poissy, France, and the Department of Immunology, Pitié-Salpétrière Hospital, Sorbonne University, France, and Rockefeller, New York, USA. St. Giles Laboratory of Infectious Diseases Human Genetics, University of Rockefeller, et al.
The study identified 19 children with a history of SARS-CoV-2 infection who exhibited multiple central nervous system (CNS) inflammatory diseases. Their symptoms include encephalopathy, cerebellar ataxia, acute disseminated encephalomyelitis (ADEM), neuromyelitis optica spectrum disorder (NMOSD), or optic neuritis.
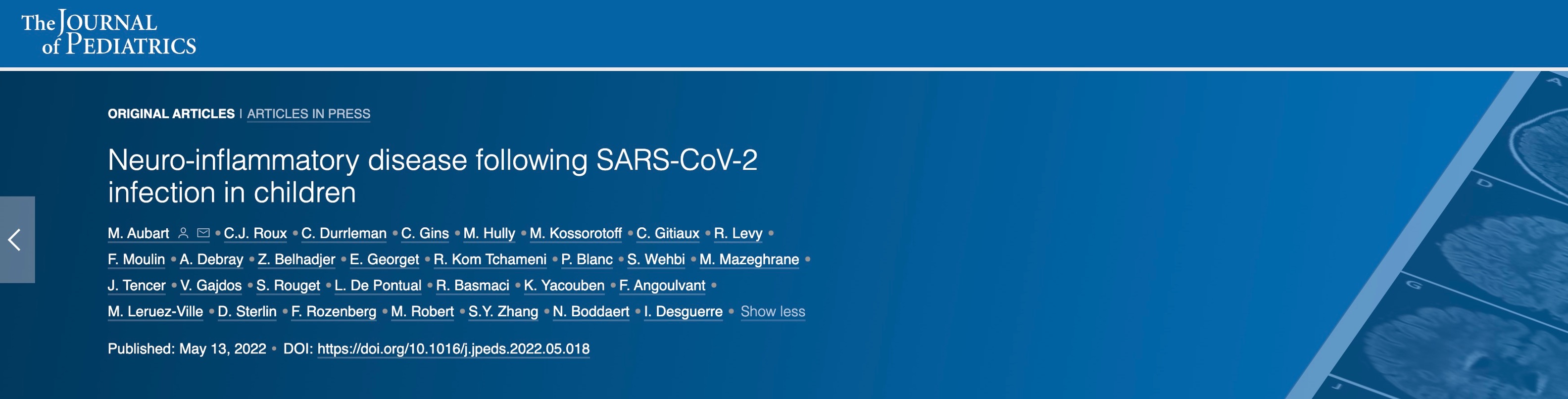
The study showed that all patients had a history of SARS-CoV-2 exposure or a positive nucleic acid test. At the time of the onset of the neurological disease, 8 children still tested positive for the new coronavirus nucleic acid (nasopharyngeal swab). Cerebrospinal fluid was abnormal in 58% of the children (11) and MRI was abnormal in 74% of the children (14).
The researchers found an "autoantibody" co-trigger in myelin-oligodendrocytes (MOG) and aquaporin 4 (AQP4) in 21 percent of the children (4 people). There were 6 children with CNS inflammation with multisystem inflammatory syndrome in children (MIS-C), but no autoimmune antibodies were found. Eighty-nine percent of patients (17) received anti-inflammatory therapy, mainly high-dose methylprednisolone injections. So far, all patients have recovered without recurrence.
Previously, clinicians found that after adults were infected with the new coronavirus, their symptoms initially mostly manifested in the respiratory system, ranging from asymptomatic infection to severe respiratory failure. But subsequently, reports of neurological complications including nonspecific headaches, delirium, dizziness and stroke have increased. Severe inflammatory central nervous system (CNS) such as encephalitis, acute disseminated encephalomyelitis (ADEM), and optic neuritis after infection are relatively rare.
Relatively speaking, the course of children infected with the new coronavirus is usually less severe, and the respiratory symptoms are milder than adults. However, multisystem inflammatory syndrome in children (MIS-C) is a unique manifestation of children infected with the new crown. It is estimated that 1-2 people will develop MIS-C for every 10,000 infected children. Some patients with MIS-C also have inflammatory diseases of the nervous system.
The researchers reviewed pediatric patients referred to the Necker-Enfantsmalades Hospital in Paris, France between January 1, 2020 and July 1, 2021, and screened 19 patients who developed central nervous system inflammation within six weeks of infection with the new coronavirus. children.
The median age of the patients was 8.7 years (1.4 years–15.3 years), and there were 12 girls and 7 boys. Before admission, all children had no previous history of serious infection, vaccine complications, or underlying neurological abnormalities. A child had a history of systemic juvenile idiopathic arthritis that had not received treatment for many years. Another child had sickle cell disease and received a bone marrow transplant 2 weeks before SARS-CoV-2 infection. None of the children had been vaccinated against SARS-Cov-2 (not yet approved at the time). Six of the 19 children did not show any symptoms of SARS-CoV-2 infection, and another 13 children developed symptoms of fever, abdominal pain, diarrhea, headache, and/or weakness (including MIS-C).
Of these, 6 children had MIS-C, 10 had cerebellar symptoms (ataxia, dizziness), and 9 had impaired cognitive function or altered consciousness. Other sporadic symptoms are loss of vision, paresthesia or hyperesthesia, sphincter disturbances, or facial paralysis. The investigators performed routine cerebrospinal fluid (CSF) testing in all patients at a median of 8 days (0 to 17 days) after the onset of neurological symptoms.
Eleven of the 19 children developed polycytosis (median 23 leukocytes/μL, maximum 300, predominantly lymphocytes or neutrophils). PCR for Listeria monocytogenes, cytomegalovirus, enterovirus, herpes simplex virus 1 and 2, human herpesvirus 6, paracholecystovirus, and varicella-zoster virus were negative in the cerebrospinal fluid of all children. Only 1 of the 19 patients had elevated protein levels, ≥50 mg/dL, on routine cerebrospinal fluid testing. CSF oligoclonal zones (gold standard for judging intrathecal immunoglobulin synthesis) were identified in 2 of 10 patients tested. Interferon alpha secretion in cerebrospinal fluid was consistently negative when tested on nine patients. Cytokines (IL1, IL6, IL10, TNF) in cerebrospinal fluid were measured in 9 patients, abnormal in 3 patients: single IL6 elevation in 2 children (1118 and 1551 pg/ml, 200 times normal) ; One child had an increase of ≤10 times normal for all 3 cytokines.
MRI abnormalities were found in 14 of 19 patients. MRI showed ADEM with multifocal brain injury in 4 cases, optic neuritis in 1 case; cytotoxic lesions of the corpus callosum (CLOCC syndrome) in 3 cases, restricted diffusion to the corpus callosum, T2-FLAIR hyperintensity, and 2 cases of the cerebellum One case showed isolated optic neuritis, isolated facial neuritis and polyneuritis, respectively. Five of the 19 spinal MRIs were abnormal: 5 showed myelitis, 3 of which were associated with ADEM, 1 was isolated, and 1 was associated with contrast enhancement of the cauda equina root. All myelitis cases showed involvement of more than 3 vertebral bodies. The serum of 4 of 10 children tested was positive for anti-MOG (myelinating oligodendrocytes) and anti-AQP4 (aquaporin 4) antibodies. The main clinical significance of AQP4 is in the diagnosis of neuromyelitis optica. The glycoprotein of MOG is the outermost membrane protein on the surface of myelin membrane and oligodendrocytes, and is a key component of demyelination in multiple sclerosis (MS). Antibodies against MOG can cause demyelination in vivo and in vitro .
The serum of 4 of 10 children tested was positive for anti-MOG (myelinating oligodendrocytes) and anti-AQP4 (aquaporin 4) antibodies. The main clinical significance of AQP4 is in the diagnosis of neuromyelitis optica. The glycoprotein of MOG is the outermost membrane protein on the surface of myelin membrane and oligodendrocytes, and is a key component of demyelination in multiple sclerosis (MS). Antibodies against MOG can cause demyelination in vivo and in vitro .
A 14-year-old anti-AQP4 antibody-positive girl with no prior significant medical history presented with isolated visual symptoms in the right eye, other neurological examinations were normal, and the clinical diagnosis was optic neuritis. Brain MRI showed optic neuritis without cerebral or spinal abnormalities. The other 3 children with positive anti-MOG antibodies were 1.5 years old, 4 years old and 10 years old, including 2 boys. None of the three cases had MIS-C symptoms, and twenty had neurological symptoms (two with ataxia and one with seizures, loss of consciousness, facial paralysis, and hemiplegia). The third patient was admitted to the intensive care unit. In fact, reports of inflammation of the nervous system caused by the new coronavirus infection have recently attracted much attention. The latest research from the University Medical Center Rotterdam in the Netherlands shows that these symptoms in patients with COVID-19 are related to the level of inflammation in the nerves of the brain. The research team tracked important brain inflammatory markers and demonstrated severe neuroinflammation in patients with COVID-19 through imaging methods.
In fact, reports of inflammation of the nervous system caused by the new coronavirus infection have recently attracted much attention. The latest research from the University Medical Center Rotterdam in the Netherlands shows that these symptoms in patients with COVID-19 are related to the level of inflammation in the nerves of the brain. The research team tracked important brain inflammatory markers and demonstrated severe neuroinflammation in patients with COVID-19 through imaging methods.  The research team from the University of Rotterdam in the Netherlands wrote in the paper "Long COVID is associated with extensive in-vivo neuroinflammation on [18F]DPA-714 PET" that although the new coronavirus mainly affects the respiratory system in the acute phase of the new crown infection, its long-term The effects are mainly on the nervous system. The most commonly reported symptoms were fatigue, loss of smell, dysgeusia, and cognitive problems. Even in patients with relatively mild initial (respiratory) symptoms, these symptoms persist for months after infection. According to data from the CDC, one in five patients with the new crown has symptoms of the new crown. However, knowledge of the pathophysiology of these debilitating symptoms and their long-term effects is still very lacking.
The research team from the University of Rotterdam in the Netherlands wrote in the paper "Long COVID is associated with extensive in-vivo neuroinflammation on [18F]DPA-714 PET" that although the new coronavirus mainly affects the respiratory system in the acute phase of the new crown infection, its long-term The effects are mainly on the nervous system. The most commonly reported symptoms were fatigue, loss of smell, dysgeusia, and cognitive problems. Even in patients with relatively mild initial (respiratory) symptoms, these symptoms persist for months after infection. According to data from the CDC, one in five patients with the new crown has symptoms of the new crown. However, knowledge of the pathophysiology of these debilitating symptoms and their long-term effects is still very lacking.
The study focused on microglia, which are phagocytic cells that colonize the brain and are antigenically enhanced, morphologically stretched, and functionally active in response to inflammatory stimuli. When inflammation occurs, microglia can rapidly proliferate, increase or re-express MHC antigens, migrate and change into a phagocyte-like form (amoeba-like) and burst to secrete a large number of cytokines and cytotoxic substances.
Microglia are distributed in all parts of the brain and are 5 times more abundant in gray matter than in white matter. There were more microglia in the hippocampus, olfactory lobe, and basal ganglia than in the thalamus and hypothalamus, but the least in the brainstem and cerebellum. Microglia are widely considered to be the main immune effectors within the central nervous system and are involved in human neurological disorders such as HIV encephalopathy, Parkinson's disease, Alzheimer's disease (senile dementia), and multiple sclerosis.
The study used positron emission tomography (PET) to observe [18F]DPA-714 levels in the brains of patients with long-term new crowns, thereby assessing the activation of inflammation by microglia in the brain nerves of patients. [18F]DPA-714 is a PET tracer, a high-affinity transporter protein (TSPO, a mitochondrial outer membrane protein expressed in activated microglia and macrophages in the brain as a marker of neuroinflammation substance) ligand. [18F]DPA-714 can be used to evaluate inflammation-specific imaging in various neuroinflammation models and brain tumor models.
The first COVID-19 patient in the University of Rotterdam study in the Netherlands was a Dutch woman in her 50s who was healthy, working full-time and living a fulfilling life before infection. She tested positive for nucleic acid in December 2020, and during the acute phase of the infection, she was not hospitalized and did not require treatment. Since the infection, she has developed severe fatigue, difficulty concentrating, anosmia and anosmia, headaches and some vision problems. Her symptoms prevented her from working, and her symptoms persisted to this day, 15 months after infection.
The second COVID-19 patient in the study was a Dutch man in his 60s who was healthy and working full-time before contracting SARS-CoV-2. He tested positive for nucleic acid in March 2020. During the acute phase of SARS-CoV-2 infection, he was hospitalized in the nursing unit for 15 days. After 10 days, he was admitted to the intensive care unit (ICU) for a day with breathing problems. During his hospital stay, he received standard medical treatment. Since the infection, he has suffered from severe fatigue and difficulty concentrating, and has been unable to work. Although things have since improved, his symptoms have persisted to this day, 24 months after infection.
The researchers performed dynamic 60-minute [18F] DPA-714 PET scans of arterial blood samples in 2 patients with long-term new crowns. To assess tracer metabolism, the researchers compared the [18F]DPA-714 metabolite in the blood of two COVID-19 patients with the metabolites in the blood of all other available subjects. They assessed activity concentrations in whole blood, corrected for injected activity and tracer maternal fraction from arterial blood samples.
The study found that [18F]DPA-714 binding in all brain regions was severely elevated in patients with COVID-19. Whole-brain gray matter quantitative BPND (=k3/k4) obtained from its 2T4k_VB model increased by an average of 121% relative to healthy control subjects. [18F]DPA-714 binding was also elevated in COVID-19 patient 2, with an average increase of 79% in whole-brain gray matter BPND (=k3/k4) obtained from the 2T4k_VB model relative to healthy control subjects.
Wang Juneng, director of the Pediatric Thoracic and Intensive Care Department of Chengda University Hospital, said that children diagnosed on the island have suffered from many neurological severe diseases, especially severe encephalopathy, acute encephalitis, and explosive cerebral edema, which are relatively rare in overseas experience. The world needs to explore the reasons behind it.
In fact, it is not "uncommon overseas experience" for children to develop encephalitis after being infected with the new coronavirus. A reporter from The Paper (www.thepaper.cn) flipped through the international journal "Journal of Pediatrics" in the field of pediatrics and found that its latest issue included a study on central nervous system inflammation in children after COVID-19 infection.
 The aforementioned study collected 19 cases of children with central nervous complications after infection with Covid-19 who were referred to the Necker-Enfants Malades Hospital from 12 hospitals in the Paris region. The research team includes the Department of Pediatric Neurology, Necker-Enfants Malades Hospital, University of Paris, France, the Department of Pediatrics, Lecoudre Louis Pasteur Hospital, France, the Department of Pediatrics, CHIPS Hospital, Poissy, France, and the Department of Immunology, Pitié-Salpétrière Hospital, Sorbonne University, France, and Rockefeller, New York, USA. St. Giles Laboratory of Infectious Diseases Human Genetics, University of Rockefeller, et al.
The aforementioned study collected 19 cases of children with central nervous complications after infection with Covid-19 who were referred to the Necker-Enfants Malades Hospital from 12 hospitals in the Paris region. The research team includes the Department of Pediatric Neurology, Necker-Enfants Malades Hospital, University of Paris, France, the Department of Pediatrics, Lecoudre Louis Pasteur Hospital, France, the Department of Pediatrics, CHIPS Hospital, Poissy, France, and the Department of Immunology, Pitié-Salpétrière Hospital, Sorbonne University, France, and Rockefeller, New York, USA. St. Giles Laboratory of Infectious Diseases Human Genetics, University of Rockefeller, et al.The study identified 19 children with a history of SARS-CoV-2 infection who exhibited multiple central nervous system (CNS) inflammatory diseases. Their symptoms include encephalopathy, cerebellar ataxia, acute disseminated encephalomyelitis (ADEM), neuromyelitis optica spectrum disorder (NMOSD), or optic neuritis.
The study showed that all patients had a history of SARS-CoV-2 exposure or a positive nucleic acid test. At the time of the onset of the neurological disease, 8 children still tested positive for the new coronavirus nucleic acid (nasopharyngeal swab). Cerebrospinal fluid was abnormal in 58% of the children (11) and MRI was abnormal in 74% of the children (14).
The researchers found an "autoantibody" co-trigger in myelin-oligodendrocytes (MOG) and aquaporin 4 (AQP4) in 21 percent of the children (4 people). There were 6 children with CNS inflammation with multisystem inflammatory syndrome in children (MIS-C), but no autoimmune antibodies were found. Eighty-nine percent of patients (17) received anti-inflammatory therapy, mainly high-dose methylprednisolone injections. So far, all patients have recovered without recurrence.
Previously, clinicians found that after adults were infected with the new coronavirus, their symptoms initially mostly manifested in the respiratory system, ranging from asymptomatic infection to severe respiratory failure. But subsequently, reports of neurological complications including nonspecific headaches, delirium, dizziness and stroke have increased. Severe inflammatory central nervous system (CNS) such as encephalitis, acute disseminated encephalomyelitis (ADEM), and optic neuritis after infection are relatively rare.
Relatively speaking, the course of children infected with the new coronavirus is usually less severe, and the respiratory symptoms are milder than adults. However, multisystem inflammatory syndrome in children (MIS-C) is a unique manifestation of children infected with the new crown. It is estimated that 1-2 people will develop MIS-C for every 10,000 infected children. Some patients with MIS-C also have inflammatory diseases of the nervous system.
The researchers reviewed pediatric patients referred to the Necker-Enfantsmalades Hospital in Paris, France between January 1, 2020 and July 1, 2021, and screened 19 patients who developed central nervous system inflammation within six weeks of infection with the new coronavirus. children.
The median age of the patients was 8.7 years (1.4 years–15.3 years), and there were 12 girls and 7 boys. Before admission, all children had no previous history of serious infection, vaccine complications, or underlying neurological abnormalities. A child had a history of systemic juvenile idiopathic arthritis that had not received treatment for many years. Another child had sickle cell disease and received a bone marrow transplant 2 weeks before SARS-CoV-2 infection. None of the children had been vaccinated against SARS-Cov-2 (not yet approved at the time). Six of the 19 children did not show any symptoms of SARS-CoV-2 infection, and another 13 children developed symptoms of fever, abdominal pain, diarrhea, headache, and/or weakness (including MIS-C).
Of these, 6 children had MIS-C, 10 had cerebellar symptoms (ataxia, dizziness), and 9 had impaired cognitive function or altered consciousness. Other sporadic symptoms are loss of vision, paresthesia or hyperesthesia, sphincter disturbances, or facial paralysis. The investigators performed routine cerebrospinal fluid (CSF) testing in all patients at a median of 8 days (0 to 17 days) after the onset of neurological symptoms.
Eleven of the 19 children developed polycytosis (median 23 leukocytes/μL, maximum 300, predominantly lymphocytes or neutrophils). PCR for Listeria monocytogenes, cytomegalovirus, enterovirus, herpes simplex virus 1 and 2, human herpesvirus 6, paracholecystovirus, and varicella-zoster virus were negative in the cerebrospinal fluid of all children. Only 1 of the 19 patients had elevated protein levels, ≥50 mg/dL, on routine cerebrospinal fluid testing. CSF oligoclonal zones (gold standard for judging intrathecal immunoglobulin synthesis) were identified in 2 of 10 patients tested. Interferon alpha secretion in cerebrospinal fluid was consistently negative when tested on nine patients. Cytokines (IL1, IL6, IL10, TNF) in cerebrospinal fluid were measured in 9 patients, abnormal in 3 patients: single IL6 elevation in 2 children (1118 and 1551 pg/ml, 200 times normal) ; One child had an increase of ≤10 times normal for all 3 cytokines.
MRI abnormalities were found in 14 of 19 patients. MRI showed ADEM with multifocal brain injury in 4 cases, optic neuritis in 1 case; cytotoxic lesions of the corpus callosum (CLOCC syndrome) in 3 cases, restricted diffusion to the corpus callosum, T2-FLAIR hyperintensity, and 2 cases of the cerebellum One case showed isolated optic neuritis, isolated facial neuritis and polyneuritis, respectively. Five of the 19 spinal MRIs were abnormal: 5 showed myelitis, 3 of which were associated with ADEM, 1 was isolated, and 1 was associated with contrast enhancement of the cauda equina root. All myelitis cases showed involvement of more than 3 vertebral bodies.
 The serum of 4 of 10 children tested was positive for anti-MOG (myelinating oligodendrocytes) and anti-AQP4 (aquaporin 4) antibodies. The main clinical significance of AQP4 is in the diagnosis of neuromyelitis optica. The glycoprotein of MOG is the outermost membrane protein on the surface of myelin membrane and oligodendrocytes, and is a key component of demyelination in multiple sclerosis (MS). Antibodies against MOG can cause demyelination in vivo and in vitro .
The serum of 4 of 10 children tested was positive for anti-MOG (myelinating oligodendrocytes) and anti-AQP4 (aquaporin 4) antibodies. The main clinical significance of AQP4 is in the diagnosis of neuromyelitis optica. The glycoprotein of MOG is the outermost membrane protein on the surface of myelin membrane and oligodendrocytes, and is a key component of demyelination in multiple sclerosis (MS). Antibodies against MOG can cause demyelination in vivo and in vitro .A 14-year-old anti-AQP4 antibody-positive girl with no prior significant medical history presented with isolated visual symptoms in the right eye, other neurological examinations were normal, and the clinical diagnosis was optic neuritis. Brain MRI showed optic neuritis without cerebral or spinal abnormalities. The other 3 children with positive anti-MOG antibodies were 1.5 years old, 4 years old and 10 years old, including 2 boys. None of the three cases had MIS-C symptoms, and twenty had neurological symptoms (two with ataxia and one with seizures, loss of consciousness, facial paralysis, and hemiplegia). The third patient was admitted to the intensive care unit.
 In fact, reports of inflammation of the nervous system caused by the new coronavirus infection have recently attracted much attention. The latest research from the University Medical Center Rotterdam in the Netherlands shows that these symptoms in patients with COVID-19 are related to the level of inflammation in the nerves of the brain. The research team tracked important brain inflammatory markers and demonstrated severe neuroinflammation in patients with COVID-19 through imaging methods.
In fact, reports of inflammation of the nervous system caused by the new coronavirus infection have recently attracted much attention. The latest research from the University Medical Center Rotterdam in the Netherlands shows that these symptoms in patients with COVID-19 are related to the level of inflammation in the nerves of the brain. The research team tracked important brain inflammatory markers and demonstrated severe neuroinflammation in patients with COVID-19 through imaging methods.  The research team from the University of Rotterdam in the Netherlands wrote in the paper "Long COVID is associated with extensive in-vivo neuroinflammation on [18F]DPA-714 PET" that although the new coronavirus mainly affects the respiratory system in the acute phase of the new crown infection, its long-term The effects are mainly on the nervous system. The most commonly reported symptoms were fatigue, loss of smell, dysgeusia, and cognitive problems. Even in patients with relatively mild initial (respiratory) symptoms, these symptoms persist for months after infection. According to data from the CDC, one in five patients with the new crown has symptoms of the new crown. However, knowledge of the pathophysiology of these debilitating symptoms and their long-term effects is still very lacking.
The research team from the University of Rotterdam in the Netherlands wrote in the paper "Long COVID is associated with extensive in-vivo neuroinflammation on [18F]DPA-714 PET" that although the new coronavirus mainly affects the respiratory system in the acute phase of the new crown infection, its long-term The effects are mainly on the nervous system. The most commonly reported symptoms were fatigue, loss of smell, dysgeusia, and cognitive problems. Even in patients with relatively mild initial (respiratory) symptoms, these symptoms persist for months after infection. According to data from the CDC, one in five patients with the new crown has symptoms of the new crown. However, knowledge of the pathophysiology of these debilitating symptoms and their long-term effects is still very lacking.The study focused on microglia, which are phagocytic cells that colonize the brain and are antigenically enhanced, morphologically stretched, and functionally active in response to inflammatory stimuli. When inflammation occurs, microglia can rapidly proliferate, increase or re-express MHC antigens, migrate and change into a phagocyte-like form (amoeba-like) and burst to secrete a large number of cytokines and cytotoxic substances.
Microglia are distributed in all parts of the brain and are 5 times more abundant in gray matter than in white matter. There were more microglia in the hippocampus, olfactory lobe, and basal ganglia than in the thalamus and hypothalamus, but the least in the brainstem and cerebellum. Microglia are widely considered to be the main immune effectors within the central nervous system and are involved in human neurological disorders such as HIV encephalopathy, Parkinson's disease, Alzheimer's disease (senile dementia), and multiple sclerosis.
The study used positron emission tomography (PET) to observe [18F]DPA-714 levels in the brains of patients with long-term new crowns, thereby assessing the activation of inflammation by microglia in the brain nerves of patients. [18F]DPA-714 is a PET tracer, a high-affinity transporter protein (TSPO, a mitochondrial outer membrane protein expressed in activated microglia and macrophages in the brain as a marker of neuroinflammation substance) ligand. [18F]DPA-714 can be used to evaluate inflammation-specific imaging in various neuroinflammation models and brain tumor models.
The first COVID-19 patient in the University of Rotterdam study in the Netherlands was a Dutch woman in her 50s who was healthy, working full-time and living a fulfilling life before infection. She tested positive for nucleic acid in December 2020, and during the acute phase of the infection, she was not hospitalized and did not require treatment. Since the infection, she has developed severe fatigue, difficulty concentrating, anosmia and anosmia, headaches and some vision problems. Her symptoms prevented her from working, and her symptoms persisted to this day, 15 months after infection.
The second COVID-19 patient in the study was a Dutch man in his 60s who was healthy and working full-time before contracting SARS-CoV-2. He tested positive for nucleic acid in March 2020. During the acute phase of SARS-CoV-2 infection, he was hospitalized in the nursing unit for 15 days. After 10 days, he was admitted to the intensive care unit (ICU) for a day with breathing problems. During his hospital stay, he received standard medical treatment. Since the infection, he has suffered from severe fatigue and difficulty concentrating, and has been unable to work. Although things have since improved, his symptoms have persisted to this day, 24 months after infection.
The researchers performed dynamic 60-minute [18F] DPA-714 PET scans of arterial blood samples in 2 patients with long-term new crowns. To assess tracer metabolism, the researchers compared the [18F]DPA-714 metabolite in the blood of two COVID-19 patients with the metabolites in the blood of all other available subjects. They assessed activity concentrations in whole blood, corrected for injected activity and tracer maternal fraction from arterial blood samples.
The study found that [18F]DPA-714 binding in all brain regions was severely elevated in patients with COVID-19. Whole-brain gray matter quantitative BPND (=k3/k4) obtained from its 2T4k_VB model increased by an average of 121% relative to healthy control subjects. [18F]DPA-714 binding was also elevated in COVID-19 patient 2, with an average increase of 79% in whole-brain gray matter BPND (=k3/k4) obtained from the 2T4k_VB model relative to healthy control subjects.

Related Posts
0 Comments
Write A Comments