The current round of monkeypox epidemics that spread around the world began in the United Kingdom, and the United Kingdom is also the country with the largest number of confirmed cases of monkeypox. On June 10, local time, the UK Health Safety Agency (UKHSA) released its first technical briefing on the monkeypox outbreak in the UK.  The report includes the latest epidemiological data on monkeypox in the UK, detailed anonymous interviews with patients, and an initial assessment of the genomic differences between the outbreak virus and previous monkeypox viruses, and will help global health agencies to better understand spread of monkeypox and targeted interventions.
The report includes the latest epidemiological data on monkeypox in the UK, detailed anonymous interviews with patients, and an initial assessment of the genomic differences between the outbreak virus and previous monkeypox viruses, and will help global health agencies to better understand spread of monkeypox and targeted interventions.
According to the report, 99% of the British monkeypox cases interviewed were males aged 30-40, and many of the patients had already started showing symptoms in April. Geographic, multi-channel sexual networks amplify the spread of monkeypox virus. Mutations occurring in the monkeypox virus genome may have implications for the function of viral proteins, including the possibility of increased resistance to the virus.
In addition, the report classifies the possible spread of the monkeypox outbreak into four levels and classifies the current situation in the UK as level 2, "transmission in a defined subgroup with a large number of close contacts". The UK Health Security Agency said it was closely monitoring for any evidence of possible escalation to level 3 - "transmission in multiple subgroups or larger subgroups".
According to the U.S. Centers for Disease Control and Prevention, as of June 11, a total of 1,472 cases of monkeypox have been confirmed worldwide, and 366 cases of monkeypox have been confirmed in the United Kingdom.
Dr Meera Chand, Director of Clinical and Emerging Infections at the UK Health Security Agency, said, "The UK government is working with global partners to advance the investigations we need to help us better understand monkeypox virus. and its spread, driving mitigation measures such as vaccines and treatments. These new data can also inform the public health response to the outbreak to further reduce transmission.”
He said many aspects of the outbreak needed further investigation. The UK Health Security Agency has now convened an expert group comprising public health, NHS and academic partners to carry out a comprehensive investigation. The results will be published in a subsequent technical briefing.
Sexual network transmission makes epidemic prevention and control challenges and opportunities coexist
Since 6 May 2022, there have been confirmed cases of monkeypox infection in the UK, the report said. As of 8 June 2022, there were 336 laboratory-confirmed cases in the UK, including 320 in England. Most of the patients had no travel history to monkeypox-endemic countries.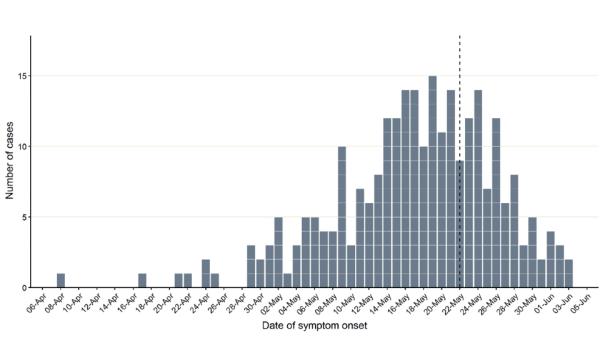
152 of the 152 cases participated in a more detailed questionnaire, and 151 of the 152 men interviewed identified themselves as gay, bisexual, and other men who have sex with men (GBMSM), or had had same-sex sexual encounters. Seventy-five cases (22%) reported recent travel abroad within the 21 days prior to symptom onset, of which 59 reported travel within Europe.
The investigators focused on the sexual health of the cases, and as of May 25, 2022, of the 82 identified cases known or suspected to be associated with sexual network transmission of GBMSM, the investigators used 45 (55%) of them. More specific and detailed questionnaires were re-interviewed.
These patients had symptom onset dates from April 8 to May 20, 2022, and all cases were confirmed in May 2022. Investigators' analysis of patient onset, travel, and date of participation in events found that 31 (69% of 45) interviewed cases who had not traveled abroad developed symptoms since April 2022.
Findings suggest monkeypox is spread through geographically dispersed sexual networks, the report noted. Almost all (98%) of the interviewed cases reported having sex with other men during the incubation period (5 to 21 days). Most (60% of 45) were diagnosed with an STI a year earlier, 44% (20 of 45) reported having more than 10 sexual partners in the first 3 months, 44% (45) 20 of the people) reported group sex during the incubation period. The sexual network involved in this outbreak covers both inside and outside the UK, with 30% (13 of 45 cases) reporting having sex in cities other than their place of residence, and 20% (9 of 45) reporting having sex outside the UK Had sex, 24% (11 of 45) reported having sex with a non-UK resident male during the incubation period.
The report pointed out that this mode of transmission will bring both challenges and opportunities to epidemic prevention and control. "Traditional contact tracing as a primary control intervention for this particular group will face difficulties as most cases report sexual contact with a new or casual partner, which is often not traceable. detail."
But on the other hand, the UK sees opportunities and possibilities for prevention and control as well: First, the UK Sexual Health Services (SHS) can be a potential environment for implementing control interventions (such as vaccines) because there are infections Contacts have been established between at-risk individuals and these service centers. For example, most of the 45 investigated cases tested negative for HIV because many of them (29 of 32) received HIV PrEP intervention at SHS, and all HIV-infected cases were in these centers receive treatment.
Second, 44% (20 of 45) of those interviewed said they had been to a sex venue in the UK or abroad, such as a sauna or sex club, during the incubation period. Therefore, working with sex sites to implement targeted interventions will aid in outbreak control.
Again, the survey revealed that the use of geospatial dating mobile apps was high among cases, with 64% (28 of 45) of cases reporting using such apps during the incubation period of their illness to meet new people mate, this suggests that these apps may also be useful platforms for disseminating health information and applying innovative approaches to contact tracing.
However, the report noted that the results of this early rapid sexual health questionnaire had some limitations. These findings may not represent a complete clearing of the outbreak, as virus transmission patterns are likely to evolve. Therefore, ongoing analysis of case interviews may indicate whether these patterns are changing.
Mutations in viral genes may lead to increased viral resistance
The UK Health Security Agency report pointed out that compared to other virus genome sequencing, monkeypox virus genome sequencing presents special difficulties.
The monkeypox virus genome consists of two deoxyribonucleic acid (DNA) strands, approximately 197 kb in length, with an average guanine-cytosine content (GC) of 33% in base pairs. The genome contains 190 coding sequences with a central region and accessory genomes at the ends of the genome, with a typical inverted repeat (about 6.5 kb in length) at each end.
The report pointed out that the special genome structure of monkeypox poses a challenge to the accurate reconstruction of the genome, and the inverted tandem repeats make it difficult to sequence using short sequence alignment (short reads) methods. The low guanine-cytosine content of the genome results in a PolyA/T structure (consecutive AT base pairs), making precise sequencing difficult. In addition, locally tandem repeats are scattered throughout the genome, which also presents challenges for sequencing.
Accurate genome reconstruction relies on coverage of sufficient depth and breadth. So far, researchers have mainly sequenced the monkeypox virus genome sequence through metagenomic sequencing methods. The feasibility of metagenomics approaches to generate useful sequences is often limited by the ratio of host-to-viral gene reads in a sample, a problem that may be partially alleviated by very in-depth sequencing.
Previously, research teams from many countries around the world have published the sequencing report of the monkeypox virus genome, and pointed out that the number of mutations in monkeypox virus nucleotides exceeds expectations. The report by the British Health and Safety Agency is the first to link the mutation of the monkeypox virus gene with the function change of the virus protein.
Compared with the monkeypox virus strain found in the UK in 2018, the current UK monkeypox virus strain contains 48 single mutations in its genome, the report said. Twenty-seven of the mutations were synonymous and did not alter viral proteins, while the other 21 resulted in changes in viral proteins.
Based on the known functions of the viral proteins, the researchers ranked these mutations as low, medium, or high priority, and the assessment was based on the impact of completely removing these proteins from the virus. But the researchers say it is not yet possible to predict the difference between a single gene mutation and a complete protein deletion.
The analysis showed that among the 21 mutations, there were 2 low-priority mutations: C9L(R48C), an interferon agonist whose ability to replicate in the presence of interferon becomes worse when deleted; A46L(H221Y ), a virulence factor that, when deleted, reduces the virulence of the virus in mice.
4 medium-priority mutations: C23L(S105L), a chemokine-binding protein, which when deleted increases disease severity in rabbits; C22L(S54F), tumor necrosis factor (TNF), which when deleted increases lung disease in mice Pathology; C19L(D266N), ankyrin repeat protein (function unknown, possibly host range or toxicity).
Among the medium-priority mutations, of particular note is F13L(E353K), the target of the antiviral drug Tecovirimat. As an antiviral drug for the treatment of smallpox, Tecovirimat is currently the only drug approved by the US FDA for the treatment of monkeypox. Studies have shown that a single mutation in F13L (G277C) will lead to the development of resistance to Tecovirimat.
There are 3 mutations in one protein that are listed as high priority: B21/B22 (D209N, P722S, M1741I): This is a T cell inhibitor also present in vaccinia virus, camelpox virus and horsepox Viruses, knocking this protein into a non-virulent vaccinia strain increased disease severity and mortality in rats.
The final report also cautiously stated that the mutated genes of this round of monkeypox virus are distributed throughout the genome, and a small number of protein mutations caused by it are related to virus transmission, toxicity or interaction with antiviral drugs, but subsequent structural modeling is required to Assess the impact of individual mutations on proteins.
In follow-up studies, the team will also examine levels of asymptomatic infection, viral dynamics, vaccine response and immunity, drug post-exposure prophylaxis, early treatment and risk of transmission, quarantine dates, media reporting behavior and bias, the report said. , the long-term consequences of infection and other aspects of further investigation.
 The report includes the latest epidemiological data on monkeypox in the UK, detailed anonymous interviews with patients, and an initial assessment of the genomic differences between the outbreak virus and previous monkeypox viruses, and will help global health agencies to better understand spread of monkeypox and targeted interventions.
The report includes the latest epidemiological data on monkeypox in the UK, detailed anonymous interviews with patients, and an initial assessment of the genomic differences between the outbreak virus and previous monkeypox viruses, and will help global health agencies to better understand spread of monkeypox and targeted interventions.According to the report, 99% of the British monkeypox cases interviewed were males aged 30-40, and many of the patients had already started showing symptoms in April. Geographic, multi-channel sexual networks amplify the spread of monkeypox virus. Mutations occurring in the monkeypox virus genome may have implications for the function of viral proteins, including the possibility of increased resistance to the virus.
In addition, the report classifies the possible spread of the monkeypox outbreak into four levels and classifies the current situation in the UK as level 2, "transmission in a defined subgroup with a large number of close contacts". The UK Health Security Agency said it was closely monitoring for any evidence of possible escalation to level 3 - "transmission in multiple subgroups or larger subgroups".
According to the U.S. Centers for Disease Control and Prevention, as of June 11, a total of 1,472 cases of monkeypox have been confirmed worldwide, and 366 cases of monkeypox have been confirmed in the United Kingdom.
Dr Meera Chand, Director of Clinical and Emerging Infections at the UK Health Security Agency, said, "The UK government is working with global partners to advance the investigations we need to help us better understand monkeypox virus. and its spread, driving mitigation measures such as vaccines and treatments. These new data can also inform the public health response to the outbreak to further reduce transmission.”
He said many aspects of the outbreak needed further investigation. The UK Health Security Agency has now convened an expert group comprising public health, NHS and academic partners to carry out a comprehensive investigation. The results will be published in a subsequent technical briefing.
Sexual network transmission makes epidemic prevention and control challenges and opportunities coexist
Since 6 May 2022, there have been confirmed cases of monkeypox infection in the UK, the report said. As of 8 June 2022, there were 336 laboratory-confirmed cases in the UK, including 320 in England. Most of the patients had no travel history to monkeypox-endemic countries.
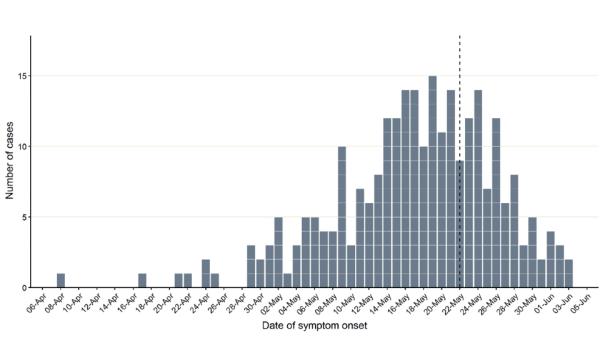
The graph above shows the number of confirmed cases of monkeypox in the UK by date of symptom onset as of 8 June 2022
Of the cases in England, 81% were London residents. When gender information was available, 311 (99% of 314) confirmed cases were male and 3 were female. The median age of confirmed cases in the UK is 38.152 of the 152 cases participated in a more detailed questionnaire, and 151 of the 152 men interviewed identified themselves as gay, bisexual, and other men who have sex with men (GBMSM), or had had same-sex sexual encounters. Seventy-five cases (22%) reported recent travel abroad within the 21 days prior to symptom onset, of which 59 reported travel within Europe.
The investigators focused on the sexual health of the cases, and as of May 25, 2022, of the 82 identified cases known or suspected to be associated with sexual network transmission of GBMSM, the investigators used 45 (55%) of them. More specific and detailed questionnaires were re-interviewed.
These patients had symptom onset dates from April 8 to May 20, 2022, and all cases were confirmed in May 2022. Investigators' analysis of patient onset, travel, and date of participation in events found that 31 (69% of 45) interviewed cases who had not traveled abroad developed symptoms since April 2022.
Findings suggest monkeypox is spread through geographically dispersed sexual networks, the report noted. Almost all (98%) of the interviewed cases reported having sex with other men during the incubation period (5 to 21 days). Most (60% of 45) were diagnosed with an STI a year earlier, 44% (20 of 45) reported having more than 10 sexual partners in the first 3 months, 44% (45) 20 of the people) reported group sex during the incubation period. The sexual network involved in this outbreak covers both inside and outside the UK, with 30% (13 of 45 cases) reporting having sex in cities other than their place of residence, and 20% (9 of 45) reporting having sex outside the UK Had sex, 24% (11 of 45) reported having sex with a non-UK resident male during the incubation period.
The report pointed out that this mode of transmission will bring both challenges and opportunities to epidemic prevention and control. "Traditional contact tracing as a primary control intervention for this particular group will face difficulties as most cases report sexual contact with a new or casual partner, which is often not traceable. detail."
But on the other hand, the UK sees opportunities and possibilities for prevention and control as well: First, the UK Sexual Health Services (SHS) can be a potential environment for implementing control interventions (such as vaccines) because there are infections Contacts have been established between at-risk individuals and these service centers. For example, most of the 45 investigated cases tested negative for HIV because many of them (29 of 32) received HIV PrEP intervention at SHS, and all HIV-infected cases were in these centers receive treatment.
Second, 44% (20 of 45) of those interviewed said they had been to a sex venue in the UK or abroad, such as a sauna or sex club, during the incubation period. Therefore, working with sex sites to implement targeted interventions will aid in outbreak control.
Again, the survey revealed that the use of geospatial dating mobile apps was high among cases, with 64% (28 of 45) of cases reporting using such apps during the incubation period of their illness to meet new people mate, this suggests that these apps may also be useful platforms for disseminating health information and applying innovative approaches to contact tracing.
However, the report noted that the results of this early rapid sexual health questionnaire had some limitations. These findings may not represent a complete clearing of the outbreak, as virus transmission patterns are likely to evolve. Therefore, ongoing analysis of case interviews may indicate whether these patterns are changing.
Mutations in viral genes may lead to increased viral resistance
The UK Health Security Agency report pointed out that compared to other virus genome sequencing, monkeypox virus genome sequencing presents special difficulties.
The monkeypox virus genome consists of two deoxyribonucleic acid (DNA) strands, approximately 197 kb in length, with an average guanine-cytosine content (GC) of 33% in base pairs. The genome contains 190 coding sequences with a central region and accessory genomes at the ends of the genome, with a typical inverted repeat (about 6.5 kb in length) at each end.
The report pointed out that the special genome structure of monkeypox poses a challenge to the accurate reconstruction of the genome, and the inverted tandem repeats make it difficult to sequence using short sequence alignment (short reads) methods. The low guanine-cytosine content of the genome results in a PolyA/T structure (consecutive AT base pairs), making precise sequencing difficult. In addition, locally tandem repeats are scattered throughout the genome, which also presents challenges for sequencing.
Accurate genome reconstruction relies on coverage of sufficient depth and breadth. So far, researchers have mainly sequenced the monkeypox virus genome sequence through metagenomic sequencing methods. The feasibility of metagenomics approaches to generate useful sequences is often limited by the ratio of host-to-viral gene reads in a sample, a problem that may be partially alleviated by very in-depth sequencing.
Previously, research teams from many countries around the world have published the sequencing report of the monkeypox virus genome, and pointed out that the number of mutations in monkeypox virus nucleotides exceeds expectations. The report by the British Health and Safety Agency is the first to link the mutation of the monkeypox virus gene with the function change of the virus protein.
Compared with the monkeypox virus strain found in the UK in 2018, the current UK monkeypox virus strain contains 48 single mutations in its genome, the report said. Twenty-seven of the mutations were synonymous and did not alter viral proteins, while the other 21 resulted in changes in viral proteins.
Based on the known functions of the viral proteins, the researchers ranked these mutations as low, medium, or high priority, and the assessment was based on the impact of completely removing these proteins from the virus. But the researchers say it is not yet possible to predict the difference between a single gene mutation and a complete protein deletion.
The analysis showed that among the 21 mutations, there were 2 low-priority mutations: C9L(R48C), an interferon agonist whose ability to replicate in the presence of interferon becomes worse when deleted; A46L(H221Y ), a virulence factor that, when deleted, reduces the virulence of the virus in mice.
4 medium-priority mutations: C23L(S105L), a chemokine-binding protein, which when deleted increases disease severity in rabbits; C22L(S54F), tumor necrosis factor (TNF), which when deleted increases lung disease in mice Pathology; C19L(D266N), ankyrin repeat protein (function unknown, possibly host range or toxicity).
Among the medium-priority mutations, of particular note is F13L(E353K), the target of the antiviral drug Tecovirimat. As an antiviral drug for the treatment of smallpox, Tecovirimat is currently the only drug approved by the US FDA for the treatment of monkeypox. Studies have shown that a single mutation in F13L (G277C) will lead to the development of resistance to Tecovirimat.
There are 3 mutations in one protein that are listed as high priority: B21/B22 (D209N, P722S, M1741I): This is a T cell inhibitor also present in vaccinia virus, camelpox virus and horsepox Viruses, knocking this protein into a non-virulent vaccinia strain increased disease severity and mortality in rats.
The final report also cautiously stated that the mutated genes of this round of monkeypox virus are distributed throughout the genome, and a small number of protein mutations caused by it are related to virus transmission, toxicity or interaction with antiviral drugs, but subsequent structural modeling is required to Assess the impact of individual mutations on proteins.
In follow-up studies, the team will also examine levels of asymptomatic infection, viral dynamics, vaccine response and immunity, drug post-exposure prophylaxis, early treatment and risk of transmission, quarantine dates, media reporting behavior and bias, the report said. , the long-term consequences of infection and other aspects of further investigation.
Related Posts
0 Comments
Write A Comments