
Studies have shown that first-time infection with the new coronavirus (SARS-CoV-2) increases the risk of illness, death, and sequelae in patients. However, whether reinfection with the new crown will further increase the risk has not been systematically studied. With at least 500 million people infected with the new crown worldwide, the Omicron variant BA.4/5 has stronger immune escape and reinfection capabilities, and research on reinfection is imminent.
Recently, Washington University School of Medicine and the St. Louis Veterans Health Care System jointly released a blockbuster study: Outcomes of SARS-CoV-2 Reinfection.
By studying a large sample of 5.69 million people, they found that re-infected people showed an increased risk of all-cause mortality, hospitalization and many diseases compared with those who were first infected with the new crown. The risk was significantly increased in people who were unvaccinated or who had one or two or more shots before a second infection.
The risk of superinfection was most pronounced in the acute phase, but persisted beyond the acute phase of reinfection, with the risk of most sequelae still evident at 6 months. Assessment of the cumulative risk of superinfection compared with an uninfected control group showed that the risk of all-cause mortality and the excess burden and risk of other diseases increased steeply with increasing number of infections. That is, the risk was lowest in those with 1 infection, increased in those with 2 infection, and highest in those with 3 or more infections.
The findings underscore the serious consequences of reinfection and the importance of preventing reinfection.
As the Covid-19 pandemic continues for three years, the question of whether a second infection poses an additional risk is important for more and more people infected with Covid-19. For people who have already been infected with COVID-19 once, continued vigilance to reduce the risk of reinfection may be important to reduce the overall risk to an individual's health, the researchers said.
Given that SARS-CoV-2 is likely to remain a global threat for years, if not decades, the team called for the urgent need for public health measures to protect people from reinfection with the new coronavirus, the researchers said. The researchers also said that pharmacological interventions are urgently needed to reduce the risk of reinfection and its adverse health consequences.
The researchers used the U.S. Department of Veterans Affairs' National Health Care Database to build a large study cohort: 257,000 first-time infections, 389,000 re-infections (two or more infections), and 5.396 million uninfected individuals. Infect a control group to estimate the risk of all-cause mortality, hospitalization rates and outcomes for a set of prespecified events and 6-month disease burden.
Studies have found that reinfection increases the lung and several extrapulmonary organ systems (cardiovascular disease, coagulation and blood system, diabetes, fatigue, gastrointestinal disease, kidney disease, mental health disorders, musculoskeletal disease) compared to people who were first infected. disease and neurological disorders) for additional risks of all-cause death, hospitalization, and adverse health outcomes.
The risk of superinfection was significant in unvaccinated people and in people who received 1 or 2 or more shots before a second infection.
A series of findings suggest that reinfection increases nontrivial risks of all-cause mortality, hospitalization, and adverse health outcomes in the acute and post-acute phases. Reinfection prevention strategies are needed to reduce the overall burden of death and disease from SARS-CoV-2.
Among those with 2019-nCoV reinfection, 36,417 (12.29%) were infected twice, 2,263 (0.76%) were infected three times, and 246 (0.08%) were infected four or more times.
In the reinfected population, the median interval between first and second infection was 79 days (48-119 days), and the median between second and third infection was 65 days (43-97 days).
Sequelae of SARS-CoV-2 Reinfection
To better understand whether reinfection increases risk, the research team first conducted an analysis: examining the risk of all-cause mortality, hospitalization, and a range of illnesses in people who were reinfected compared to people who were first-time infected with Covid-19.
The research team provided two risk measures: (1) the hazard ratio (HR, Hazard Ratio) of re-infected people compared to first-time infection (2) the excess disease burden per 1,000 people after new crown re-infection compared to first-time infection . The excess disease burden per 1,000 people, specifically, is an estimate of the excess number of patients compared with the baseline of the corresponding disease incidence per 1,000 people in the reference group.
Compared with the first-time infection of the new crown, the all-cause mortality rate of the new crown re-infected within 6 months increased, the hazard ratio was 2.14 times that of the first-time infection (95%CI: 1.97, 2.33), and the excess all-cause death per 1,000 people 23.8 people died (95%CI: 18.9, 29.2); the risk of hospitalization was also increased in reinfected patients, with a hazard ratio of 2.98 times that of first-time infection (95%CI: 2.83, 3.12), and the excess hospitalization burden per 1,000 people was 95.47 (95% confidence interval: 89.17, 102.03), and the hazard ratio of at least one sequelae of SARS-CoV-2 infection was 1.82 times (95% confidence interval: 1.78, 1.88), and the excess sequelae burden per thousand people was 196.2 ( 95% confidence interval: 186.57, 205.87).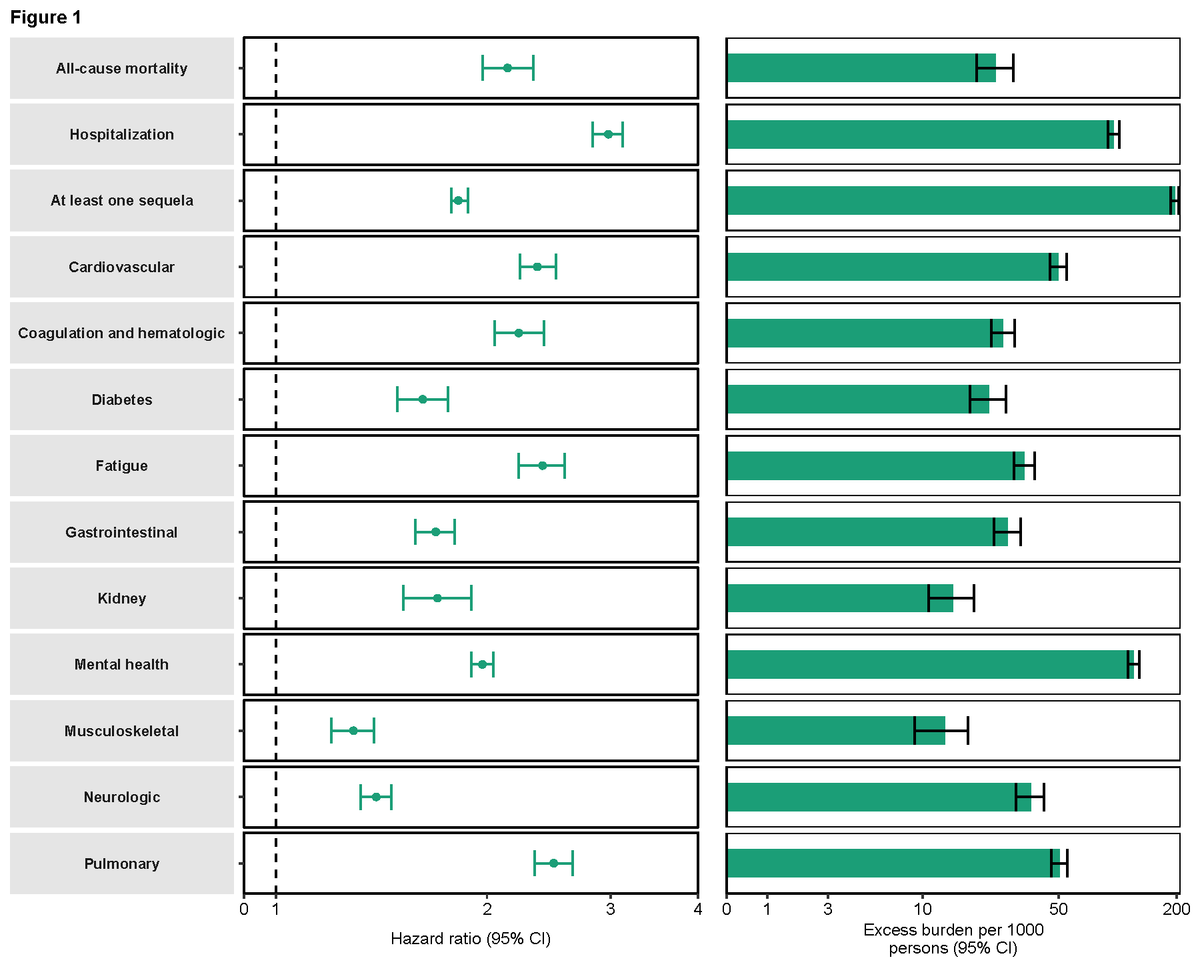
 Compared with the first-time infection, the hazard ratio of the new crown reinfected person to develop lung disease was 2.49 times; the excess burden of lung disease per 1,000 people was 50.35.
Compared with the first-time infection, the hazard ratio of the new crown reinfected person to develop lung disease was 2.49 times; the excess burden of lung disease per 1,000 people was 50.35.
The hazard ratio for several extrapulmonary organ system diseases, including cardiovascular disease, was 2.36 times; the excess disease burden per 1,000 people was 49.83.
The hazard ratio for coagulation and blood system was 2.22 times; the excess burden per thousand people was 25.93.
Hazard ratio for fatigue was 2.4 times; excess burden per thousand people was 33.39
The hazard ratio for gastrointestinal diseases was 1.69 times, and the excess burden was 27.45 per 1,000 people.
The hazard ratio for kidney disease was 1.70 times; the excess disease burden per 1,000 people was 14.31.
The hazard ratio for mental health disorders was 1.97 times, and the excess disease burden per 1,000 people was 121.05.
The hazard ratio for diabetes was 1.62 times, and the excess disease burden per 1,000 people was 21.98.
The hazard ratio for musculoskeletal disease was 1.29 times, and the excess disease burden per 1,000 people was 12.97.
The hazard ratio for neurological diseases was 1.39 times, and the excess disease burden per 1,000 people was 36.02.
Risk remains evident 6 months after reinfection
The research team further analyzed whether the sequelae risk of SARS-CoV-2 reinfection existed in the acute and post-acute phases of reinfection. To this end, the research team examined disease risk and burden every 30 days from the time of reinfection to 180 days. Compared with first-time infections, re-infected persons exhibited a risk of all-cause mortality, hospitalization, and at least one sequelae, and excess disease burden in both the acute and post-acute phases.
The risk and excess burden of all-cause death, hospitalization, and at least one sequelae in the post-acute phase diminished over time, but the increased risk remained significant even six months after reinfection. Examination of organ system sequelae showed increased hazard ratios and excess disease burden in all organ systems during the acute phase; disease risk and excess burden persisted in the acute phase of reinfection, and most remained evident 6 months after reinfection.
Examination of organ system sequelae showed increased hazard ratios and excess disease burden in all organ systems during the acute phase; disease risk and excess burden persisted in the acute phase of reinfection, and most remained evident 6 months after reinfection.  Cumulative risk and disease burden of two, three or more SARS-CoV-2 infections
Cumulative risk and disease burden of two, three or more SARS-CoV-2 infections
To better understand the cumulative risk posed by multiple infections, the research team assessed the absence of reinfection within 6 months of the acute phase of the first infection, i.e. those with only one infection, two infections, three or more infections the risk of infected individuals, and compared with uninfected controls.
Compared with the uninfected control group, those with only one infection had a hazard ratio of 1.35 times (95% confidence interval: 1.4, 1.36) for at least one sequelae; 84.13 excess disease burden per 1,000 people (95% confidence interval: 95% confidence interval: 82.03, 86.24); the hazard ratio of 2 infections was higher, 2.11 times (95% confidence interval: 2.07, 2.15), and the excess disease burden per 1,000 people was 234.58 (95% confidence interval: 227.08, 241.92), 3 times The hazard ratio was the highest among those with 3 or more infections, reaching 3.00 times (95% confidence interval: 2.71, 3.31); the excess disease burden per 1,000 people was 362.82 (95% confidence interval: 326.37, 398.08).
Compared with single-infection patients, the risk increase ratio of at least one sequelae in patients with secondary infection was 1.57 times (95% confidence interval: 1.53, 1.60); the excess disease burden per thousand people was 150.36 (95% confidence interval: 142.95) , 157.79); compared with those with secondary infection, the risk of at least one sequelae increased by at least 1.42 times (95% confidence interval: 1.28, 1.57) for those who were infected three or more times (95% confidence interval: 1.28, 1.57); the excess disease burden per 1,000 people was 128.33 (95% Confidence interval: 91.88, 164.31)). All-cause mortality, hospitalization rates, and sequelae were consistent by organ system examination.
Recently, Washington University School of Medicine and the St. Louis Veterans Health Care System jointly released a blockbuster study: Outcomes of SARS-CoV-2 Reinfection.
By studying a large sample of 5.69 million people, they found that re-infected people showed an increased risk of all-cause mortality, hospitalization and many diseases compared with those who were first infected with the new crown. The risk was significantly increased in people who were unvaccinated or who had one or two or more shots before a second infection.
The risk of superinfection was most pronounced in the acute phase, but persisted beyond the acute phase of reinfection, with the risk of most sequelae still evident at 6 months. Assessment of the cumulative risk of superinfection compared with an uninfected control group showed that the risk of all-cause mortality and the excess burden and risk of other diseases increased steeply with increasing number of infections. That is, the risk was lowest in those with 1 infection, increased in those with 2 infection, and highest in those with 3 or more infections.
The findings underscore the serious consequences of reinfection and the importance of preventing reinfection.
As the Covid-19 pandemic continues for three years, the question of whether a second infection poses an additional risk is important for more and more people infected with Covid-19. For people who have already been infected with COVID-19 once, continued vigilance to reduce the risk of reinfection may be important to reduce the overall risk to an individual's health, the researchers said.
Given that SARS-CoV-2 is likely to remain a global threat for years, if not decades, the team called for the urgent need for public health measures to protect people from reinfection with the new coronavirus, the researchers said. The researchers also said that pharmacological interventions are urgently needed to reduce the risk of reinfection and its adverse health consequences.
The researchers used the U.S. Department of Veterans Affairs' National Health Care Database to build a large study cohort: 257,000 first-time infections, 389,000 re-infections (two or more infections), and 5.396 million uninfected individuals. Infect a control group to estimate the risk of all-cause mortality, hospitalization rates and outcomes for a set of prespecified events and 6-month disease burden.
Studies have found that reinfection increases the lung and several extrapulmonary organ systems (cardiovascular disease, coagulation and blood system, diabetes, fatigue, gastrointestinal disease, kidney disease, mental health disorders, musculoskeletal disease) compared to people who were first infected. disease and neurological disorders) for additional risks of all-cause death, hospitalization, and adverse health outcomes.
The risk of superinfection was significant in unvaccinated people and in people who received 1 or 2 or more shots before a second infection.
A series of findings suggest that reinfection increases nontrivial risks of all-cause mortality, hospitalization, and adverse health outcomes in the acute and post-acute phases. Reinfection prevention strategies are needed to reduce the overall burden of death and disease from SARS-CoV-2.
Among those with 2019-nCoV reinfection, 36,417 (12.29%) were infected twice, 2,263 (0.76%) were infected three times, and 246 (0.08%) were infected four or more times.
In the reinfected population, the median interval between first and second infection was 79 days (48-119 days), and the median between second and third infection was 65 days (43-97 days).
Sequelae of SARS-CoV-2 Reinfection
To better understand whether reinfection increases risk, the research team first conducted an analysis: examining the risk of all-cause mortality, hospitalization, and a range of illnesses in people who were reinfected compared to people who were first-time infected with Covid-19.
The research team provided two risk measures: (1) the hazard ratio (HR, Hazard Ratio) of re-infected people compared to first-time infection (2) the excess disease burden per 1,000 people after new crown re-infection compared to first-time infection . The excess disease burden per 1,000 people, specifically, is an estimate of the excess number of patients compared with the baseline of the corresponding disease incidence per 1,000 people in the reference group.
Compared with the first-time infection of the new crown, the all-cause mortality rate of the new crown re-infected within 6 months increased, the hazard ratio was 2.14 times that of the first-time infection (95%CI: 1.97, 2.33), and the excess all-cause death per 1,000 people 23.8 people died (95%CI: 18.9, 29.2); the risk of hospitalization was also increased in reinfected patients, with a hazard ratio of 2.98 times that of first-time infection (95%CI: 2.83, 3.12), and the excess hospitalization burden per 1,000 people was 95.47 (95% confidence interval: 89.17, 102.03), and the hazard ratio of at least one sequelae of SARS-CoV-2 infection was 1.82 times (95% confidence interval: 1.78, 1.88), and the excess sequelae burden per thousand people was 196.2 ( 95% confidence interval: 186.57, 205.87).
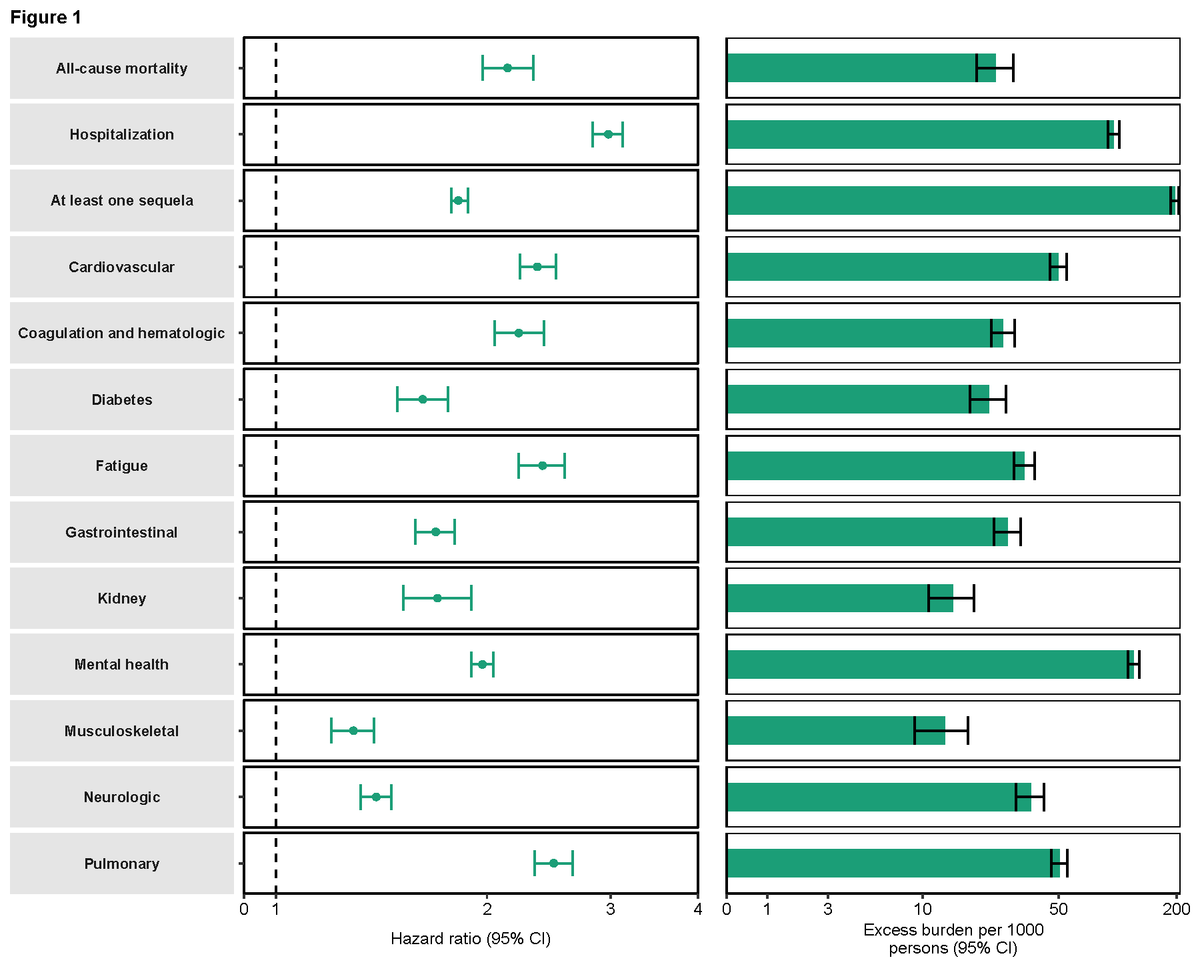
 Compared with the first-time infection, the hazard ratio of the new crown reinfected person to develop lung disease was 2.49 times; the excess burden of lung disease per 1,000 people was 50.35.
Compared with the first-time infection, the hazard ratio of the new crown reinfected person to develop lung disease was 2.49 times; the excess burden of lung disease per 1,000 people was 50.35.The hazard ratio for several extrapulmonary organ system diseases, including cardiovascular disease, was 2.36 times; the excess disease burden per 1,000 people was 49.83.
The hazard ratio for coagulation and blood system was 2.22 times; the excess burden per thousand people was 25.93.
Hazard ratio for fatigue was 2.4 times; excess burden per thousand people was 33.39
The hazard ratio for gastrointestinal diseases was 1.69 times, and the excess burden was 27.45 per 1,000 people.
The hazard ratio for kidney disease was 1.70 times; the excess disease burden per 1,000 people was 14.31.
The hazard ratio for mental health disorders was 1.97 times, and the excess disease burden per 1,000 people was 121.05.
The hazard ratio for diabetes was 1.62 times, and the excess disease burden per 1,000 people was 21.98.
The hazard ratio for musculoskeletal disease was 1.29 times, and the excess disease burden per 1,000 people was 12.97.
The hazard ratio for neurological diseases was 1.39 times, and the excess disease burden per 1,000 people was 36.02.
Risk remains evident 6 months after reinfection
The research team further analyzed whether the sequelae risk of SARS-CoV-2 reinfection existed in the acute and post-acute phases of reinfection. To this end, the research team examined disease risk and burden every 30 days from the time of reinfection to 180 days. Compared with first-time infections, re-infected persons exhibited a risk of all-cause mortality, hospitalization, and at least one sequelae, and excess disease burden in both the acute and post-acute phases.
The risk and excess burden of all-cause death, hospitalization, and at least one sequelae in the post-acute phase diminished over time, but the increased risk remained significant even six months after reinfection.
 Examination of organ system sequelae showed increased hazard ratios and excess disease burden in all organ systems during the acute phase; disease risk and excess burden persisted in the acute phase of reinfection, and most remained evident 6 months after reinfection.
Examination of organ system sequelae showed increased hazard ratios and excess disease burden in all organ systems during the acute phase; disease risk and excess burden persisted in the acute phase of reinfection, and most remained evident 6 months after reinfection.  Cumulative risk and disease burden of two, three or more SARS-CoV-2 infections
Cumulative risk and disease burden of two, three or more SARS-CoV-2 infectionsTo better understand the cumulative risk posed by multiple infections, the research team assessed the absence of reinfection within 6 months of the acute phase of the first infection, i.e. those with only one infection, two infections, three or more infections the risk of infected individuals, and compared with uninfected controls.
Compared with the uninfected control group, those with only one infection had a hazard ratio of 1.35 times (95% confidence interval: 1.4, 1.36) for at least one sequelae; 84.13 excess disease burden per 1,000 people (95% confidence interval: 95% confidence interval: 82.03, 86.24); the hazard ratio of 2 infections was higher, 2.11 times (95% confidence interval: 2.07, 2.15), and the excess disease burden per 1,000 people was 234.58 (95% confidence interval: 227.08, 241.92), 3 times The hazard ratio was the highest among those with 3 or more infections, reaching 3.00 times (95% confidence interval: 2.71, 3.31); the excess disease burden per 1,000 people was 362.82 (95% confidence interval: 326.37, 398.08).
Compared with single-infection patients, the risk increase ratio of at least one sequelae in patients with secondary infection was 1.57 times (95% confidence interval: 1.53, 1.60); the excess disease burden per thousand people was 150.36 (95% confidence interval: 142.95) , 157.79); compared with those with secondary infection, the risk of at least one sequelae increased by at least 1.42 times (95% confidence interval: 1.28, 1.57) for those who were infected three or more times (95% confidence interval: 1.28, 1.57); the excess disease burden per 1,000 people was 128.33 (95% Confidence interval: 91.88, 164.31)). All-cause mortality, hospitalization rates, and sequelae were consistent by organ system examination.

Related Posts
0 Comments
Write A Comments