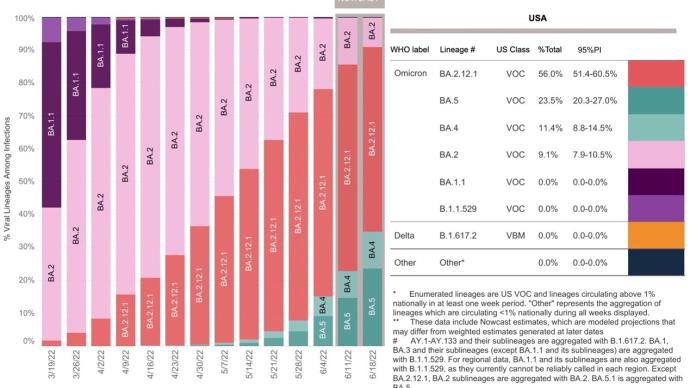
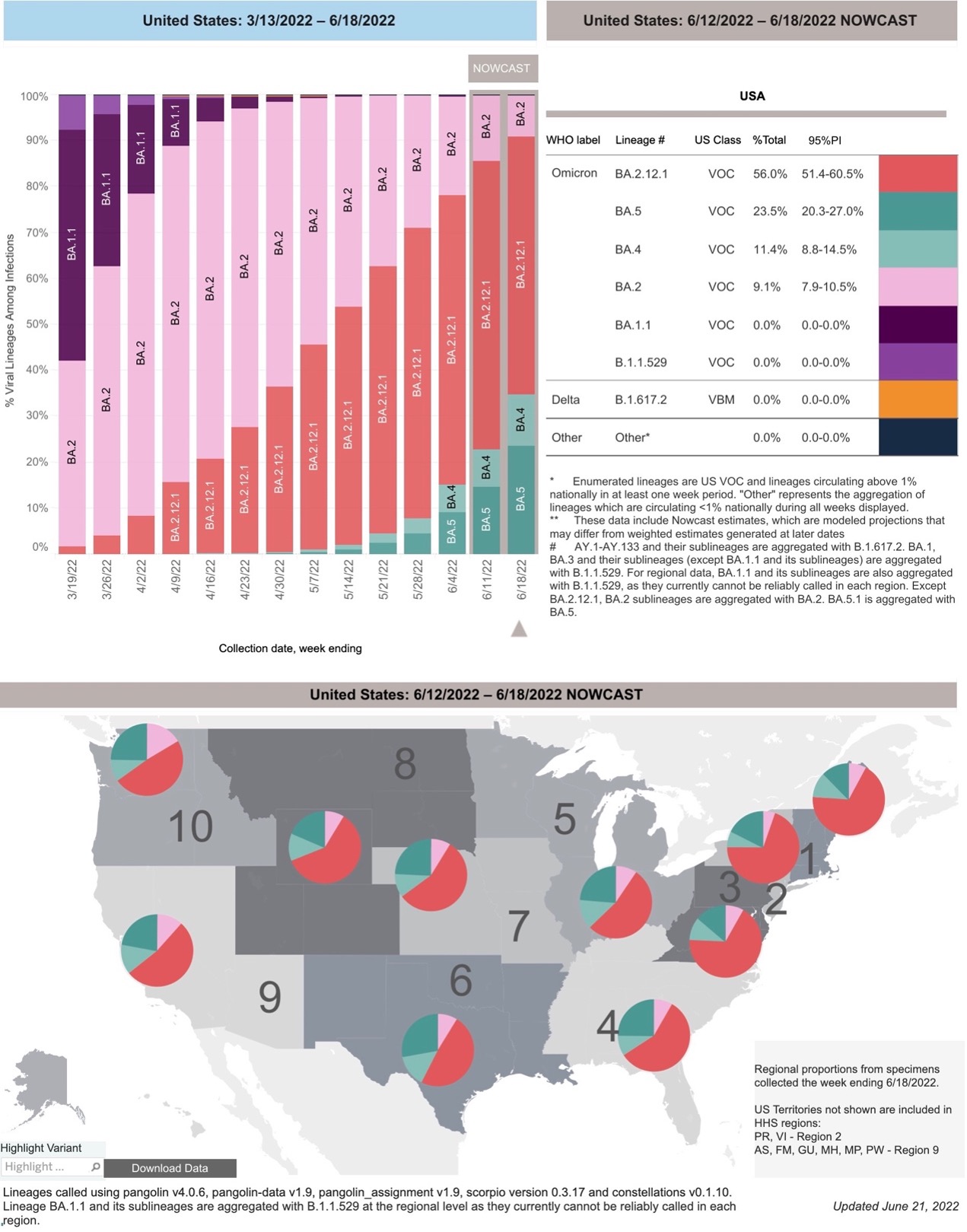
 New Omicron variants, BA.2.12.1, BA.4 and BA.5, are dominating the United States. In particular, BA.4 and BA.5 surged by 61.57% within a week, accounting for 34.9% of new cases in the United States.
New Omicron variants, BA.2.12.1, BA.4 and BA.5, are dominating the United States. In particular, BA.4 and BA.5 surged by 61.57% within a week, accounting for 34.9% of new cases in the United States. 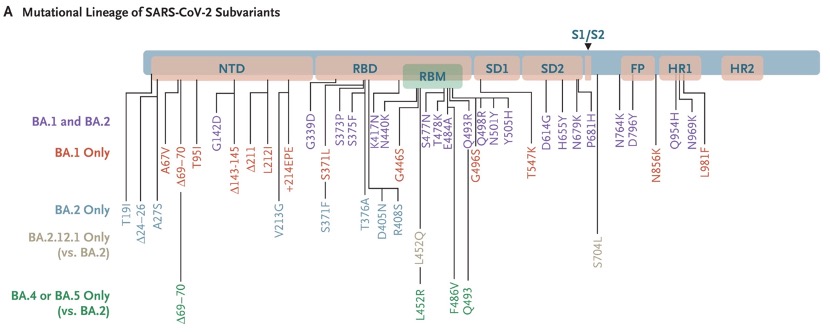 What is the immune escape ability of Omicron BA.2.12.1, BA.4 and BA.5? On June 22, local time, the New England Journal of Medicine (NEJM), an international authoritative academic journal, published the latest research from Harvard Beth Israel Deaconess Medical Center. The study found that after 2 weeks of inoculation with 3 injections of mRNA vaccine (BNT162b2), the neutralizing antibody titer of the subjects against BA.4/5 decreased by 21 times compared with the original strain of the new coronavirus.
What is the immune escape ability of Omicron BA.2.12.1, BA.4 and BA.5? On June 22, local time, the New England Journal of Medicine (NEJM), an international authoritative academic journal, published the latest research from Harvard Beth Israel Deaconess Medical Center. The study found that after 2 weeks of inoculation with 3 injections of mRNA vaccine (BNT162b2), the neutralizing antibody titer of the subjects against BA.4/5 decreased by 21 times compared with the original strain of the new coronavirus.At the same time, this study also showed that BA.2.12.1, BA.4 and BA.5 were also able to escape the immunity brought about by infection with BA.1 and BA.2. This study provides support for why BA.2.12.1, BA.4 and BA.5 can cause breakthrough infection (infection after vaccination) and superinfection.
Specifically, in this study, the Harvard Beth Israel Deaconess Medical Center tested neutralizing antibody titers of the original strain, BA.1, BA.2, BA.2.12.1, and BA.4 or BA.5 . The study was divided into two cohorts, the vaccine cohort, in which 27 participants were vaccinated with mRNA vaccine (BNT162b2); the infection cohort, in which 27 participants were infected with BA.1 or BA.2, and the median duration of infection was 29 days ( 2 days to 113 days).
In the vaccine cohort, participants were excluded if they had a history of SARS-CoV-2 infection or were positive for antibodies, or if they had received another Covid-19 vaccine or immunosuppressive drug.
Six months after the first two mRNA immunizations, subjects had a median neutralizing antibody pseudovirus titer of 124, but all tested groups (original SARS-CoV-2, BA.1, BA.2, The titers of BA.2.12.1 and BA.4 or BA.5) were all less than 20.
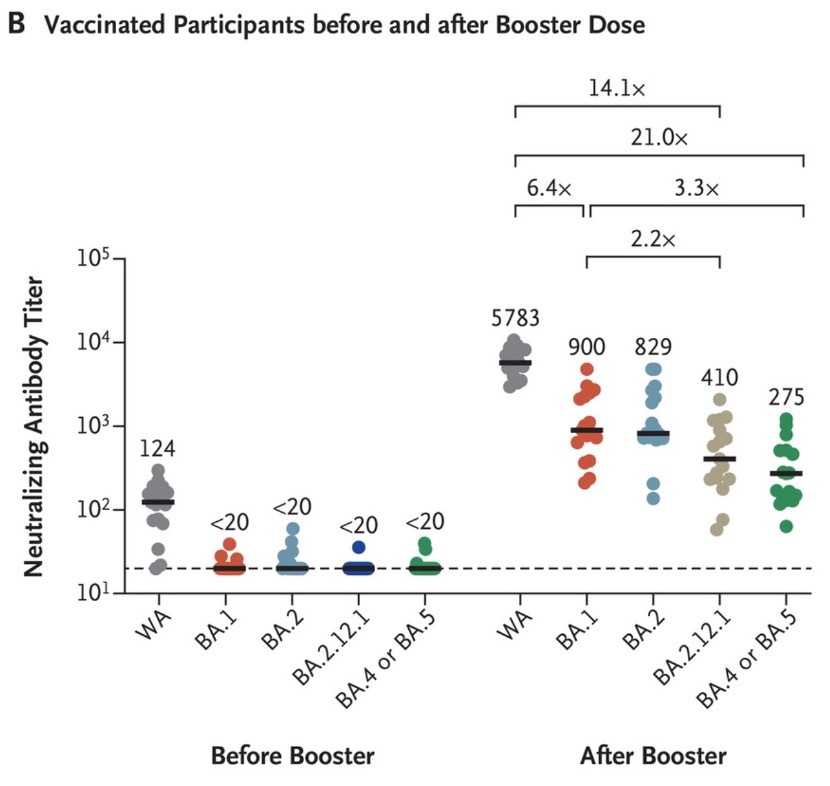 After 2 weeks of receiving the booster, participants' median neutralizing antibody titers increased substantially to 5783 against the original strain, 900 against BA.1, 829 against BA.2, and 410 against BA.2.12.1 , 275 for BA.4 and 275 for BA.5. These data show that, compared with the original strain of 2019-nCoV, in vivo neutralizing antibody titers decreased by 6.4 times to BA.1, 7.0 times to BA.2, and 14.1 times to BA.2.1 after inoculation with 3 injections of mRNA. , 21.0 times lower for BA.4 or BA.5. In addition, compared with the neutralizing antibody titers of BA.1, the median titer of BA.2.12.1 was reduced by 2.2-fold, and the BA.4 or BA.5 subvariant was reduced by 3.3-fold.
After 2 weeks of receiving the booster, participants' median neutralizing antibody titers increased substantially to 5783 against the original strain, 900 against BA.1, 829 against BA.2, and 410 against BA.2.12.1 , 275 for BA.4 and 275 for BA.5. These data show that, compared with the original strain of 2019-nCoV, in vivo neutralizing antibody titers decreased by 6.4 times to BA.1, 7.0 times to BA.2, and 14.1 times to BA.2.1 after inoculation with 3 injections of mRNA. , 21.0 times lower for BA.4 or BA.5. In addition, compared with the neutralizing antibody titers of BA.1, the median titer of BA.2.12.1 was reduced by 2.2-fold, and the BA.4 or BA.5 subvariant was reduced by 3.3-fold.Of the participants infected with Omicron BA.1 or BA.2, all but one were vaccinated against Covid-19. Due to differences in sampling after infection onset, some samples may not reflect peak neutralizing antibody titers. Among subjects with a history of Covid-19, the median neutralizing antibody titers against the original strain of 2019-nCoV were 11050, 1740 against BA.1, 1910 against BA.2, and 1910 against BA.2.12.1 For 1150, it becomes 590 for BA.4/5 sub.
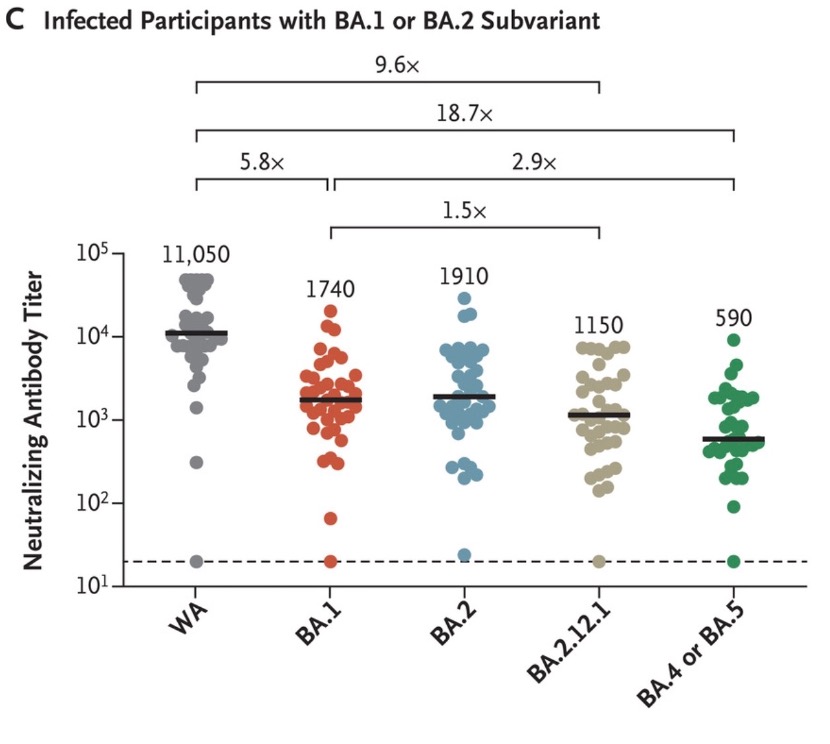 These data show that, compared with the original strain of the new coronavirus, the neutralizing antibody titers to BA.1 were reduced by 6.4 times, 5.8 times to BA.2, 9.6 times to BA.2.12.1, and 9.6 times to BA. .4/5 is 18.7 times lower. In addition, compared to the median neutralizing antibody titers for BA.1, there was a 1.5-fold reduction for BA.2.12.1 and a 2.9-fold reduction for BA.4 or BA.5.
These data show that, compared with the original strain of the new coronavirus, the neutralizing antibody titers to BA.1 were reduced by 6.4 times, 5.8 times to BA.2, 9.6 times to BA.2.12.1, and 9.6 times to BA. .4/5 is 18.7 times lower. In addition, compared to the median neutralizing antibody titers for BA.1, there was a 1.5-fold reduction for BA.2.12.1 and a 2.9-fold reduction for BA.4 or BA.5.These data suggest that BA.2.12.1, BA.4 and BA.5 essentially escape the neutralizing antibodies induced by vaccination and infection, the researchers said. In addition, neutralizing antibody titers against BA.4 or BA.5 and neutralizing antibody titers against BA.2.12.1 were lower than those against BA.1 and BA.2, suggesting that Omicron's New variants continue to develop in the direction of immune escape. These findings provide a reference for the immunological background of BA.2.12.1, BA.4 and BA.5 in populations with high vaccination frequency and BA.1 or BA.2 infection.
BA.2.12.1, BA.4, BA.5 mutations at the L452 site of the spike protein are the spikes that the Omicron BA.1 and BA.2 sub-variants do not have, but the delta variant has. protein mutation sites. The difference is that the mutation of BA.2.12.1 is L452Q, and the mutation of BA.4/5 is L452R. Delta is also an L452R.
This means that under strong positive selection pressure, the Omicron variant has convergent evolution with the delta strain on the spike protein gene. The mutation on the spike protein is particularly noteworthy because the spike protein plays a key role in the entry of the new coronavirus into human cells: the spike protein can bind to the ACE2 receptor of human cells, invade across the cell membrane, and open the cell door. It is also the main target of mRNA vaccine and antibody drug design.
Studies have shown that first-time infection with the new coronavirus (SARS-CoV-2) increases the risk of illness, death, and sequelae in patients. However, whether reinfection with the new crown will further increase the risk has not been systematically studied. With at least 500 million people infected with the new crown worldwide, the Omicron variant BA.4/5 has stronger immune escape and reinfection capabilities, and research on reinfection is imminent.
Recently, Washington University School of Medicine and the St. Louis Veterans Health Care System jointly released a blockbuster study: Outcomes of SARS-CoV-2 Reinfection.
By studying a large sample of 5.69 million people, they found that re-infected people showed an increased risk of all-cause mortality, hospitalization and many diseases compared with those who were first infected with the new crown. The risk was significantly increased in people who were unvaccinated or who had one or two or more shots before a second infection.
The risk of superinfection was most pronounced in the acute phase, but persisted beyond the acute phase of reinfection, with the risk of most sequelae still evident at 6 months. Assessment of the cumulative risk of superinfection compared with an uninfected control group showed that the risk of all-cause mortality and the excess burden and risk of other diseases increased steeply with increasing number of infections. That is, the risk was lowest in those with 1 infection, increased in those with 2 infection, and highest in those with 3 or more infections.
Related Posts
0 Comments
Write A Comments